Obesity hypoventilation syndrome (OHS)
Pickwickian syndrome
Obesity hypoventilation syndrome (OHS) is a condition in some obese people in which poor breathing leads to lower oxygen and higher carbon dioxide levels in the blood.
Causes
The exact cause of OHS is not known. Doctors believe OHS results from a defect in the brain's control over breathing. Excess weight against the chest wall also makes it harder for the muscles to draw in a deep breath and to breathe quickly enough. As a result, the blood contains too much carbon dioxide and not enough oxygen.
Symptoms
The main symptoms of OHS are due to lack of sleep and include:
- Poor sleep quality
-
Sleep apnea
Sleep apnea
Obstructive sleep apnea (OSA) is a problem in which your breathing pauses during sleep. This occurs because of narrowed or blocked airways.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Daytime sleepiness
-
Depression
Depression
Depression may be described as feeling sad, blue, unhappy, miserable, or down in the dumps. Most of us feel this way at one time or another for shor...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Headaches
- Tiredness
Symptoms of low blood oxygen level (chronic hypoxia) can also occur. Symptoms include shortness of breath or feeling tired after very little effort.
Exams and Tests
People with OHS are usually very overweight. A physical exam may reveal:
-
Bluish color in the lips, fingers, toes, or skin (
cyanosis
)
Cyanosis
Cyanosis is a bluish color to the skin or mucous membrane that is usually due to a lack of oxygen in the blood.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Reddish skin
-
Signs of right-sided heart failure (
cor pulmonale
), such as swollen legs or feet, shortness of breath, or feeling tired after little effort
Cor pulmonale
Cor pulmonale is a condition that causes the right side of the heart to fail. Long-term high blood pressure in the arteries of the lung and right ve...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Signs of excessive sleepiness
Tests used to help diagnose and confirm OHS include:
-
Arterial blood gas
Arterial blood gas
Blood gases are a measurement of how much oxygen and carbon dioxide are in your blood. They also determine the acidity (pH) of your blood.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Chest x-ray or CT scan to rule out other possible causes
- Lung function tests (pulmonary function tests)
-
Sleep study (polysomnography)
Sleep study (polysomnography)
Polysomnography is a sleep study. This test records certain body functions as you sleep, or try to sleep. Polysomnography is used to diagnose sleep...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Doctors can tell OHS from obstructive sleep apnea because a person with OHS has a high carbon dioxide level in their blood when awake.
Treatment
Treatment involves breathing assistance using special machines (mechanical ventilation). Options include:
-
Noninvasive mechanical ventilation such as
continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPAP)
through a mask that fits tightly over the nose or nose and mouth (mainly for sleep)
Continuous positive airway pressure (CP...
CPAP stands for continuous positive airway pressure. CPAP pumps air under pressure into the airway of the lungs, keeping the windpipe open during sl...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Oxygen therapy
-
Breathing help through an opening in the neck (
tracheostomy
) for severe cases.
Tracheostomy
A tracheostomy is a surgical procedure to create an opening through the neck into the trachea (windpipe). A tube is usually placed through this open...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment is started in the hospital or as an outpatient.
Other treatments are aimed at weight loss, which can reverse OHS.
Outlook (Prognosis)
Untreated, OHS can lead to serious heart and blood vessel problems, severe disability, or death.
Possible Complications
OHS complications related to a lack of sleep may include:
- Depression, agitation, irritability
- Increased risk of accidents or mistakes at work
- Problems with intimacy and sex
OHS can also cause heart problems, such as:
-
High blood pressure (
hypertension
)
Hypertension
Blood pressure is a measurement of the force exerted against the walls of your arteries as your heart pumps blood to your body. Hypertension is the ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Right-sided heart failure (cor pulmonale)
-
High blood pressure in the lungs (
pulmonary hypertension
)
Pulmonary hypertension
Pulmonary hypertension is high blood pressure in the arteries of the lungs. It makes the right side of the heart work harder than normal.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
When to Contact a Medical Professional
Call your health care provider if you are very tired during the day or have any other symptoms that suggest OHS.
Prevention
Maintain a healthy weight and avoid obesity. Use your CPAP or BiPAP treatment as your provider prescribed.
References
Balachandran JS, Masa JF, Mokhlesi B. Obesity hypoventilation syndrome epidemiology and diagnosis. Sleep Med Clin . 2014;9:341–347. PMC4210766 www.ncbi.nlm.nih.gov/pmc/articles/PMC4210766/ .
Malhotra A, Powell F. Disorders of ventilatory control. In: Goldman L, Schafer AI, eds. Goldman's Cecil Medicine . 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 86.
-
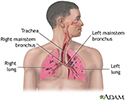
Respiratory system - illustration
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Respiratory system
illustration
Review Date: 8/11/2015
Reviewed By: Denis Hadjiliadis, MD, MHS, Associate Professor of Medicine, Pulmonary, Allergy, and Critical Care, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.