Wolff-Parkinson-White syndrome (WPW)
Preexcitation syndrome; WPW; Tachycardia - Wolff-Parkinson-White syndrome; Arrhythmia - WPW; Abnormal heart rhythm - WPW; Rapid heartbeat - WPW
Wolff-Parkinson-White (WPW) syndrome is a condition in which there is an extra electrical pathway in the heart. The condition can lead to periods of rapid heart rate ( tachycardia ).
Tachycardia
A bounding pulse is a strong throbbing felt over one of the arteries in the body. It is due to a forceful heartbeat.

WPW syndrome is one of the most common causes of fast heart rate problems in infants and children.
Causes
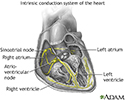
Normally, electrical signals follow a certain pathway through the heart. This helps the heart beat regularly. This prevents the heart from having extra beats or beats happening too soon.
In people with WPW syndrome, some of the heart's electrical signals go down an extra pathway. This may cause a very rapid heart rate called supraventricular tachycardia.
Most people with WPW syndrome do not have any other heart problems. However, this condition has been linked with other cardiac conditions, such as Ebstein anomaly . A form of the condition also runs in families.
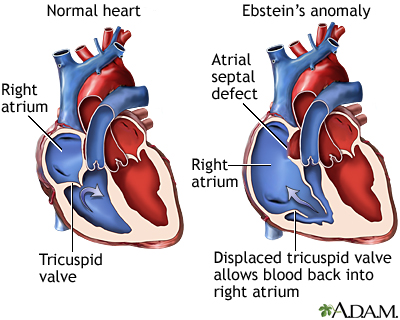
Ebstein anomaly
Ebstein anomaly is a rare heart defect in which parts of the tricuspid valve are abnormal. The tricuspid valve separates the right lower heart chamb...

Symptoms
How often a rapid heart rate occurs varies depending on the person. Some people with WPW syndrome have only a few episodes of rapid heart rate. Others may have the rapid heart rate once or twice a week or more. Also, there may be no symptoms at all, so that condition is found when a heart test is done for another reason.
A person with this syndrome may have:
-
Chest pain
or chest tightness
Chest pain
Chest pain is discomfort or pain that you feel anywhere along the front of your body between your neck and upper abdomen.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Dizziness
Dizziness
Dizziness is a term that is often used to describe 2 different symptoms: lightheadedness and vertigo. Lightheadedness is a feeling that you might fai...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Lightheadedness
Lightheadedness
Dizziness is a term that is often used to describe 2 different symptoms: lightheadedness and vertigo. Lightheadedness is a feeling that you might fai...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Fainting
Fainting
Fainting is a brief loss of consciousness due to a drop in blood flow to the brain. The episode most often lasts less than a couple of minutes and y...
Read Article Now Book Mark Article -
Palpitations
(a sensation of feeling your heart beating, usually quickly or irregularly)
Palpitations
Palpitations are feelings or sensations that your heart is pounding or racing. They can be felt in your chest, throat, or neck. You may:Have an unpl...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Shortness of breath
Shortness of breath
Breathing difficulty may involve:Difficult breathingUncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Exams and Tests
A physical exam done during a tachycardia episode will show a heart rate faster than 100 beats per minute. A normal heart rate is 60 to 100 beats per minute in adults, and under 150 beats per minute in newborns, infants, and small children. Blood pressure will be normal or low in most cases.
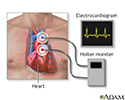
If the person is not having tachycardia at the time of the exam, the results may be normal. The condition may be diagnosed with an ECG or with continuous or person triggered ambulatory ECG monitoring, such as a Holter monitor .
Holter monitor
A Holter monitor is a machine that continuously records the heart's rhythms. The monitor is worn for 24 to 48 hours during normal activity.

A test called an electrophysiologic study ( EPS ) is done using catheters that are placed in the heart. This test may help identify the location of the extra electrical pathway.
EPS
Intracardiac electrophysiology study (EPS) is a test to look at how well the heart's electrical signals are working. It is used to check for abnorma...

Treatment
Medicines, particularly antiarrhythmic drugs such as procainamide or amiodarone, may be used to control or prevent a rapid heartbeat.
If the heart rate does not return to normal with medical treatment, doctors may use a type of therapy called electrical cardioversion (shock).
Cardioversion
Cardioversion is a method to return an abnormal heart rhythm back to normal.

The long-term treatment for WPW syndrome is very often catheter ablation . This procedure involves inserting a tube (catheter) into a vein through a small cut near the groin up to the heart area. When the tip reaches the heart, the small area that is causing the fast heart rate is destroyed using a special type of energy called radiofrequency or by freezing it (cryoablation).
Catheter ablation
Cardiac ablation is a procedure that is used to scar small areas in your heart that may be involved in your heart rhythm problems. This can prevent ...
Open heart surgery to burn or freeze the extra pathway may also provide a permanent cure for WPW syndrome. In most cases, this procedure is done only if you need heart surgery for other reasons.
Open heart surgery
Heart surgery is any surgery done on the heart muscle, valves, arteries, or the aorta and other large arteries connected to the heart. The term "ope...

Outlook (Prognosis)
Catheter ablation cures this disorder in most people. The success rate for the procedure ranges between 85% to 95%. Success rates will vary depending on the location and number of extra pathways.
Possible Complications
Complications may include:
- Complications of surgery
-
Heart failure
Heart failure
Heart failure is a condition in which the heart is no longer able to pump oxygen-rich blood to the rest of the body efficiently. This causes symptom...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Reduced blood pressure (caused by
rapid heart rate
)
Rapid heart rate
A bounding pulse is a strong throbbing felt over one of the arteries in the body. It is due to a forceful heartbeat.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Side effects of medicines
The most severe form of a rapid heartbeat is ventricular fibrillation (VF), which may rapidly lead to shock or death. It can sometimes occur in people with WPW, particularly if they also have atrial fibrillation (AF) , which is another type of abnormal heart rhythm. This type of rapid heartbeat requires emergency treatment and a procedure called cardioversion.
Ventricular fibrillation
Ventricular fibrillation (VF) is a severely abnormal heart rhythm (arrhythmia) that is life threatening.

Atrial fibrillation (AF)
Atrial fibrillation or flutter is a common type of abnormal heartbeat. The heart rhythm is fast and most often irregular.

When to Contact a Medical Professional
Call your health care provider if:
- You have symptoms of WPW syndrome.
- You have this disorder and symptoms get worse or do not improve with treatment.
Talk to your provider about whether your family members should be screened for inherited forms of this condition.
References
Olgin JE, Zipes DP. Specific arrhythmias: diagnosis and treatment. In: Mann DL, Zipes DP, Libby P, Bonow RO, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine . 10th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 37.
Van Hare GF. Disturbances of rate and rhythm of the heart. In: Kliegman RM, Stanton BF, St Geme JW, Schor NF, eds. Nelson Textbook of Pediatrics . 20th ed. Philadelphia, PA: Elsevier; 2016:chap 435.
Zimetbaum P. Cardiac arrhythmias with supraventricular origin. In: Goldman L, Schafer AI, eds. Goldman's Cecil Medicine . 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 64.
-
Cardiac conduction system disorders - overview
Animation
-
Ebstein's anomaly - illustration
Ebstein's anomaly is a congenital heart condition which results in an abnormality of the tricuspid valve. In this condition the tricuspid valve is elongated and displaced downward towards the right ventricle. The abnormality causes the tricuspid valve to leak blood backwards into the right atrium.
Ebstein's anomaly
illustration
-
Holter heart monitor - illustration
During a heart Holter monitor study, the patient wears a monitor that records electrical activity of their heart (similarly to the recording of an electrocardiogram). This usually occurs for 24 hours, while at the same time the patient also records a diary of their activity. Health care providers then analyze the recording, tabulate a report of the heart’s activity, and correlate irregular heart activity with the entries of the patient’s diary.
Holter heart monitor
illustration
-
Conduction system of the heart - illustration
The intrinsic conduction system sets the basic rhythm of the beating heart by generating impulses which stimulate the heart to contract.
Conduction system of the heart
illustration
-
Ebstein's anomaly - illustration
Ebstein's anomaly is a congenital heart condition which results in an abnormality of the tricuspid valve. In this condition the tricuspid valve is elongated and displaced downward towards the right ventricle. The abnormality causes the tricuspid valve to leak blood backwards into the right atrium.
Ebstein's anomaly
illustration
-
Holter heart monitor - illustration
During a heart Holter monitor study, the patient wears a monitor that records electrical activity of their heart (similarly to the recording of an electrocardiogram). This usually occurs for 24 hours, while at the same time the patient also records a diary of their activity. Health care providers then analyze the recording, tabulate a report of the heart’s activity, and correlate irregular heart activity with the entries of the patient’s diary.
Holter heart monitor
illustration
-
Conduction system of the heart - illustration
The intrinsic conduction system sets the basic rhythm of the beating heart by generating impulses which stimulate the heart to contract.
Conduction system of the heart
illustration
Review Date: 2/24/2016
Reviewed By: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.