Deep vein thrombosis
DVT; Blood clot in the legs; Thromboembolism; Post-phlebitic syndrome; Post-thrombotic syndrome; Venous - DVT
Deep vein thrombosis (DVT) is a condition that occurs when a blood clot forms in a vein deep inside a part of the body. It mainly affects the large veins in the lower leg and thigh, but can occur in other deep veins such as in the arms and pelvis.
Causes
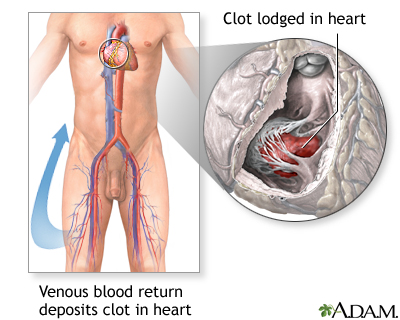
DVT is most common in adults over age 60. But it can occur at any age. When a clot breaks off and moves through the bloodstream, it is called an embolism. An embolism can get stuck in the blood vessels in the brain, lungs, heart, or another area, leading to severe damage.
Blood clots may form when something slows or changes the flow of blood in the veins. Risk factors include:
Blood clots
Blood clots are clumps that occur when blood hardens from a liquid to a solid. A blood clot that forms inside one of your veins or arteries is calle...

- A pacemaker catheter that has been passed through the vein in the groin
- Bed rest or sitting in 1 position for too long, such as plane travel
- Family history of blood clots
- Fractures in the pelvis or legs
- Giving birth within the last 6 months
- Pregnancy
-
Obesity
Obesity
Obesity means having too much body fat. It is not the same as being overweight, which means weighing too much. A person may be overweight from extr...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Recent surgery (most commonly hip, knee, or female pelvic surgery)
-
Too many blood cells being made by the bone marrow, causing the blood to be thicker than normal (
polycythemia vera
)
Polycythemia vera
Polycythemia vera is a bone marrow disease that leads to an abnormal increase in the number of blood cells. The red blood cells are mostly affected....
Read Article Now Book Mark Article - Having an indwelling (long-term) catheter in a blood vessel
Blood is more likely to clot in someone who has certain problems or disorders, such as:
- Cancer
-
Certain
autoimmune disorders
, such as
lupus
Autoimmune disorders
An autoimmune disorder occurs when the body's immune system attacks and destroys healthy body tissue by mistake. There are more than 80 types of aut...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleLupus
Systemic lupus erythematosus (SLE) is an autoimmune disease. In this disease, the body's immune system mistakenly attacks healthy tissue. It can af...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Cigarette smoking
- Conditions that make it more likely to develop blood clots
- Taking estrogens or birth control pills (this risk is even higher with smoking)
Sitting for long periods when traveling can increase the risk for DVT. This is most likely when you also have 1 or more of the risk factors listed above.
Symptoms
DVT mainly affects the large veins in the lower leg and thigh, most often on 1 side of the body. The clot can block blood flow and cause:
- Changes in skin color (redness)
- Leg pain
- Leg swelling (edema)
- Skin that feels warm to the touch
Exams and Tests
Your health care provider will perform a physical exam. The exam may show a red, swollen, or tender leg.
The 2 tests that are often done first to diagnose a DVT are:
-
D-dimer blood test
D-dimer blood test
D-dimer tests are used to check for blood clotting problems. Blood clots can cause health problems, such as:Deep vein thrombosis (DVT)Pulmonary embo...
Read Article Now Book Mark Article -
Doppler ultrasound exam
of the area of concern
Doppler ultrasound exam
This test uses ultrasound to look at the blood flow in the large arteries and veins in the arms and legs.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Blood tests may be done to check if you have an increased chance of blood clotting, including:
- Activated protein C resistance (checks for the Factor V Leiden mutation)
- Antithrombin levels
- Antiphospholipid antibodies
-
Complete blood count
(CBC)
Complete blood count
A complete blood count (CBC) test measures the following:The number of red blood cells (RBC count)The number of white blood cells (WBC count)The tota...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Genetic testing to look for mutations that make you more likely to develop blood clots, such as the prothrombin G20210A mutation
-
Lupus anticoagulant
Lupus anticoagulant
Lupus anticoagulants are antibodies against substances in the lining of cells. These substances prevent blood clotting in a test tube. They are cal...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Protein C
and
protein S
levels
Protein C
Protein C is a normal substance in the body that prevents blood clotting. A blood test can be done to see how much of this protein you have in your ...
Read Article Now Book Mark ArticleProtein S
Protein S is a normal substance in your body that prevents blood clotting. A blood test can be done to see how much of this protein you have in your...
Read Article Now Book Mark Article
Treatment
Your provider will give you medicine to thin your blood (called an anticoagulant). This will keep more clots from forming or old ones from getting bigger.
Heparin is often the first drug you will receive.
- If heparin is given through a vein (IV), you must stay in the hospital. However, most people can be treated without staying in the hospital.
- Newer forms of heparin can be given by injection under your skin once or twice a day. You may not need to stay in the hospital as long, or at all, if you are prescribed this newer form of heparin.
Depending on your medical history, a drug called fondaparinux may be recommended by your doctor as an alternative to heparin.
A blood thinning drug, for example warfarin (Coumadin), is often started along with heparin. Examples of other drugs that may be prescribed include rivaroxaban, apixaban, dabigatran, and edoxaban. Your doctor will decide which medicine is right for you.
- These drugs are taken by mouth. It takes several days to fully work.
- Heparin is not stopped until the drug has been at the right dose for at least 2 days.
- You will most likely take the blood thinner for at least 3 months. Some people must take it longer, or even for the rest of their lives, depending on their risk for another clot.
When you are taking a blood thinning drug , you are more likely to bleed, even from activities you have always done. If you are taking a blood thinner at home :
If you are taking a blood thinner at ho...
Warfarin is a medicine that makes your blood less likely to form clots. This may be important if:You have already had blood clots in your leg, arm, ...
- Take the medicine just the way your doctor prescribed it.
- Ask the doctor what to do if you miss a dose.
- Get blood tests as advised by your doctor to make sure you are taking the right dose. These tests are usually needed with warfarin.
- Learn how to take other medicines and when to eat.
- Find out how to watch for problems caused by the drug.
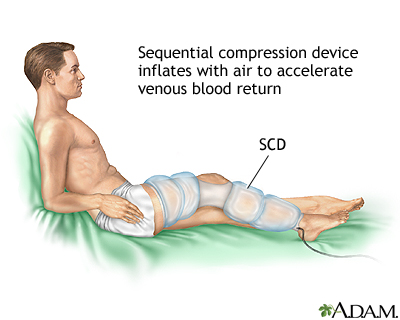
You will be told to wear a pressure (compression) stocking on your leg or legs. A pressure stocking improves blood flow in your legs and reduces your risk for complications from blood clots. It is important to wear it every day.
Pressure (compression) stocking
Compression hose; Pressure stockings; Support stockings; Gradient stockings; Varicose veins - compression stockings; Venous insufficiency - compressi...

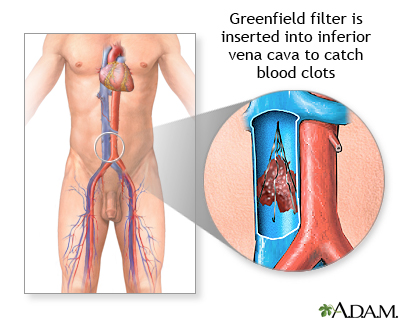
In rare cases, you may need surgery if medicines do not work. Surgery may involve:
- Placing a filter in the body's largest vein to prevent blood clots from traveling to the lungs
- Removing a large blood clot from the vein or injecting clot-busting medicines
Follow any other instructions you are given to treat your DVT.
Instructions
DVT - discharge; Blood clot in the legs - discharge; Thromboembolism - discharge; Venous thromboembolism - deep vein thrombosis; Post-phlebitic syndr...

Outlook (Prognosis)
DVT often goes away without a problem, but the condition can return. Some people may have long-term pain and swelling in the leg called post-phlebitic syndrome.
You may also have pain and changes in skin color. These symptoms can appear right away or you may not develop them for 1 or more years afterward. Wearing compression stockings during and after the DVT may help prevent this problem.
Blood clots in the thigh are more likely to break off and travel to the lungs ( pulmonary embolus ) than blood clots in the lower leg or other parts of the body.
Pulmonary embolus
A pulmonary embolus is a blockage of an artery in the lungs. The most common cause of the blockage is a blood clot.

When to Contact a Medical Professional
Call your provider if you have symptoms of DVT.
Go to the emergency room or call the local emergency number (such as 911) if you have DVT and you develop:
-
Chest pain
Chest pain
Chest pain is discomfort or pain that you feel anywhere along the front of your body between your neck and upper abdomen.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Coughing up blood
-
Difficulty breathing
Difficulty breathing
Breathing difficulty may involve:Difficult breathingUncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Fainting
Fainting
Fainting is a brief loss of consciousness due to a drop in blood flow to the brain. The episode most often lasts less than a couple of minutes and y...
Read Article Now Book Mark Article -
Loss of consciousness
Loss of consciousness
Decreased alertness is a state of reduced awareness. A coma is a state of decreased alertness from which a person cannot be awakened. A long-term co...
Read Article Now Book Mark Article - Other severe symptoms
Prevention
To prevent deep vein thrombosis:
- Wear the pressure stockings your doctor prescribed.
- Moving your legs often during long plane trips, car trips, and other situations in which you are sitting or lying down for long periods.
- Take blood thinning medicines your doctor prescribes.
-
DO NOT smoke. Talk to your doctor if you need help
quitting
.
Quitting
There are many ways to quit smoking. There are also resources to help you. Family members, friends, and co-workers may be supportive. But to be su...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
References
Guyatt GH, Akl EA, Crowther M, et al. Executive summary: antithrombotic therapy and prevention of thrombosis. 9th ed. American College of Chest Physicians evidence-based clinical practice guidelines. Chest . 2012;141(2 suppl):7S-47S. PMID: 22315257 www.ncbi.nlm.nih.gov/pubmed/22315257 .
Kline JA. Pulmonary embolism and deep vein thrombosis. In: Marx JA, Hockberger RS, Walls RM, et al, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice . 8th ed. Philadelphia, PA: Elsevier Saunders; 2014:chap 88.
-
Deep venous thrombosis, ileofemoral - illustration
This picture shows a red and swollen thigh and leg caused by a blood clot (thrombus) in the deep veins in the groin (iliofemoral veins) which prevents normal return of blood from the leg to the heart.
Deep venous thrombosis, ileofemoral
illustration
-
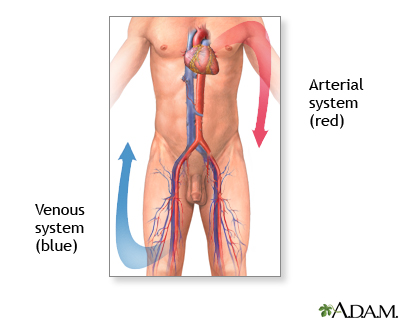
Deep veins - illustration
Veins in the extremities carry blood to the heart and lungs, where the blood is oxygenated. As the blood returns to the heart from the lungs, the arteries carry the oxygen-rich blood out to the body.
Deep veins
illustration
-
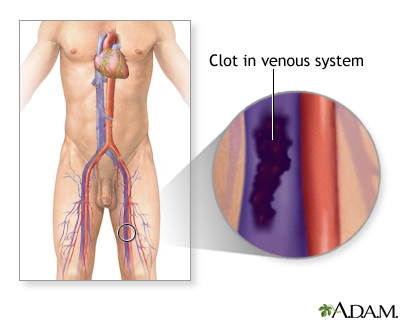
Venous blood clot - illustration
Deep venous thrombosis (DVT) affects mainly the veins in the lower leg and the thigh. It involves the formation of a clot (thrombus) in the larger veins of the area.
Venous blood clot
illustration
-
Deep veins - illustration
Veins in the extremities carry blood to the heart and lungs, where the blood is oxygenated. As the blood returns to the heart from the lungs, the arteries carry the oxygen-rich blood out to the body.
Deep veins
illustration
-
Venous thrombosis - series
Presentation
-
Deep venous thrombosis, ileofemoral - illustration
This picture shows a red and swollen thigh and leg caused by a blood clot (thrombus) in the deep veins in the groin (iliofemoral veins) which prevents normal return of blood from the leg to the heart.
Deep venous thrombosis, ileofemoral
illustration
-
Deep veins - illustration
Veins in the extremities carry blood to the heart and lungs, where the blood is oxygenated. As the blood returns to the heart from the lungs, the arteries carry the oxygen-rich blood out to the body.
Deep veins
illustration
-
Venous blood clot - illustration
Deep venous thrombosis (DVT) affects mainly the veins in the lower leg and the thigh. It involves the formation of a clot (thrombus) in the larger veins of the area.
Venous blood clot
illustration
-
Deep veins - illustration
Veins in the extremities carry blood to the heart and lungs, where the blood is oxygenated. As the blood returns to the heart from the lungs, the arteries carry the oxygen-rich blood out to the body.
Deep veins
illustration
-
Venous thrombosis - series
Presentation
Review Date: 2/7/2016
Reviewed By: Laura J. Martin, MD, MPH, ABIM Board Certified in Internal Medicine and Hospice and Palliative Medicine, Atlanta, GA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.