Bladder cancer
Transitional cell carcinoma of the bladder; Urothelial cancer
Bladder cancer is a cancer that starts in the bladder. The bladder is the body part that holds and releases urine. It is in the center of the lower abdomen.
Causes
In the United States, bladder cancer often starts from the cells lining the bladder. These cells are called transitional cells.
These tumors are classified by the way they grow:
- Papillary tumors look like warts and are attached to a stalk.
-
Nonpapillary (sessile) tumors are flat. They are much less common. But they are more
invasive
and have a worse outcome.
Invasive
An invasive disease is one that spreads to surrounding tissues. An invasive procedure is one in which the body is "invaded", or entered by a needle,...
Read Article Now Book Mark Article
The exact cause of bladder cancer is not known. But several things may make you more likely to develop it:
- Cigarette smoking: Smoking greatly increases the risk of developing bladder cancer. Up to half of all bladder cancers in men and several in women may be caused by cigarette smoke.
- Chemical exposure at work: About 1 in 4 cases of bladder cancer is caused by coming into contact with cancer-causing chemicals at work. These chemicals are called carcinogens. Dye workers, rubber workers, aluminum workers, leather workers, truck drivers, and pesticide applicators are at the highest risk.
- Chemotherapy: The chemotherapy drug cyclophosphamide may increase the risk for bladder cancer. Your doctor may prescribe a medicine to reduce this risk.
- Radiation treatment: Women who had radiation therapy to treat cervical cancer have an increased risk of developing bladder cancer.
-
Bladder infection
: A long-term (chronic) bladder infection or irritation may lead to a certain type of bladder cancer.
Bladder infection
A urinary tract infection, or UTI, is an infection of the urinary tract. The infection can occur at different points in the urinary tract, including...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Research has not shown clear evidence that using artificial sweeteners leads to bladder cancer.
Symptoms
Symptoms of bladder cancer can include:
-
Abdominal pain
Abdominal pain
Abdominal pain is pain that you feel anywhere between your chest and groin. This is often referred to as the stomach region or belly.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Blood in the urine
Blood in the urine
Blood in your urine is called hematuria. The amount may be very small and only detected with urine tests or under a microscope. In other cases, the...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Bone pain or tenderness
if the cancer spreads to the bone
Bone pain or tenderness
Bone pain or tenderness is aching or other discomfort in one or more bones.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Fatigue
-
Painful urination
Painful urination
Painful urination is any pain, discomfort, or burning sensation when passing urine.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Urinary frequency and urgency
Urinary frequency and urgency
Frequent urination means needing to urinate more often than usual. Urgent urination is a sudden, strong urge to urinate. This causes a discomfort i...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Urine leakage (incontinence)
Urine leakage (incontinence)
Urinary (or bladder) incontinence happens when you are not able to keep urine from leaking out of your urethra. The urethra is the tube that carries...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Weight loss
Weight loss
Unexplained weight loss is a decrease in body weight, when you did not try to lose the weight on your own. Many people gain and lose weight. Uninten...
Read Article Now Book Mark Article
Other diseases and conditions can cause similar symptoms. It is important to see a doctor to rule out all other possible causes.
Exams and Tests
The health care provider will perform a physical examination , including a rectal and pelvic exam.
Physical examination
During a physical examination, a health care provider studies your body to determine if you do or do not have a physical problem. A physical examinat...
Tests that may be done include:
-
Abdominal CT scan
Abdominal CT scan
An abdominal CT scan is an imaging method. This test uses x-rays to create cross-sectional pictures of the belly area. CT stands for computed tomog...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Abdominal MRI scan
-
Cystoscopy
(examining the inside of the bladder with a camera), with biopsy
Cystoscopy
Cystoscopy is a surgical procedure. This is performed to see the inside of the bladder and urethra using a telescope.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Intravenous pyelogram - IVP
Intravenous pyelogram - IVP
An intravenous pyelogram (IVP) is a special x-ray exam of the kidneys, bladder, and ureters (the tubes that carry urine from the kidneys to the bladd...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Pelvic CT scan
-
Urinalysis
Urinalysis
Urinalysis is the physical, chemical, and microscopic examination of urine. It involves a number of tests to detect and measure various compounds th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Urine cytology
Urine cytology
A cytology exam of urine is a test used to detect cancer and other diseases of the urinary tract.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
If tests confirm you have bladder cancer, additional tests will be done to see if the cancer has spread. This is called staging. Staging helps guide future treatment and follow-up and gives you some idea of what to expect in the future.
The TNM (tumor, nodes, metastatis) staging system is used to stage bladder cancer:
- Ta: The cancer is in the lining of the bladder only and has not spread.
- T1: The cancer goes through the bladder lining, but does not reach the bladder muscle.
- T2: The cancer spreads to the bladder muscle.
- T3: The cancer spreads past the bladder into the fatty tissue surrounding it.
- T4: The cancer has spread to nearby structures such as the prostate gland, uterus, vagina, rectum, abdominal wall, or pelvic wall.
Tumors are also grouped based on how they appear under a microscope. This is called grading the tumor. A high-grade tumor is fast growing and more likely to spread. Bladder cancer can spread into nearby areas, including the:
- Lymph nodes in the pelvis
- Bones
- Liver
- Lungs
Treatment
Treatment depends on the stage of the cancer, the severity of your symptoms, and your overall health.
Stage 0 and I treatments:
- Surgery to remove the tumor without removing the rest of the bladder
-
Chemotherapy
or immunotherapy placed directly into the bladder
Chemotherapy
The term chemotherapy is used to describe cancer-killing drugs. Chemotherapy may be used to:Cure the cancerShrink the cancerPrevent the cancer from ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Stage II and III treatments:
- Surgery to remove the entire bladder (radical cystectomy) and nearby lymph nodes
- Surgery to remove only part of the bladder, followed by radiation and chemotherapy
- Chemotherapy to shrink the tumor before surgery
- A combination of chemotherapy and radiation (in people who choose not to have surgery or who cannot have surgery)
Most people with stage IV tumors cannot be cured and surgery is not appropriate. In these people, chemotherapy is often considered.
CHEMOTHERAPY
Chemotherapy may be given to people with stage II and III disease either before or after surgery to help prevent the tumor from returning.
For early disease (stages 0 and I), chemotherapy is usually given directly into the bladder.
A Foley catheter can be used to deliver the medicine into the bladder. Common side effects include bladder wall irritation and pain when urinating. For more advanced stages (II-IV), chemotherapy is usually given by vein (intravenously).
Foley catheter
A urinary catheter is a tube placed in the body to drain and collect urine from the bladder.
IMMUNOTHERAPY
Bladder cancers are often treated with immunotherapy. In this treatment, a medicine triggers your immune system to attack and kill the cancer cells. Immunotherapy for bladder cancer is often performed using the Bacille Calmette-Guerin vaccine (commonly known as BCG).
As with all treatments, side effects are possible. Ask your doctor what side effects you might expect, and what to do if they occur.
SURGERY
Surgery for bladder cancer includes:
- Transurethral resection of the bladder (TURB): Cancerous bladder tissue is removed through the urethra.
- Partial or complete removal of the bladder: Many people with stage II or III bladder cancer may need to have their bladder removed (radical cystectomy). Sometimes, only part of the bladder is removed. Chemotherapy is usually given before or after this surgery.
Surgery may also be done to help your body drain urine after the bladder is removed. This may include:
- Ileal conduit: A small urine reservoir is surgically created from a short piece of your small intestine. The ureters that drain urine from the kidneys are attached to 1 end of this piece. The other end is brought out through an opening in the skin (a stoma). The stoma allows the person to drain the collected urine out of the reservoir.
- Continent urinary reservoir: A pouch to collect urine is created inside your body using a piece of your intestine. You will need to insert a tube into an opening in your skin (stoma) into this pouch to drain the urine.
- Orthotopic neobladder: This surgery is becoming more common in people who have had their bladder removed. A part of your bowel is folded over to make a pouch that collects urine. It is attached to the place in the body where the urine normally empties from the bladder. This procedure allows you to maintain some normal urinary control.
Support Groups
You can ease the stress of illness by joining a cancer support group . Sharing with others who have common experiences and problems can help you not feel alone.
Cancer support group
The following organizations are good resources for information on cancer:American Cancer Society -- www. cancer. orgCancerCare -- www. cancercare. or...
Outlook (Prognosis)
After treatment for bladder cancer, you will be closely monitored by a doctor. This may include:
- CT scans to check for the spread or return of cancer
- Monitoring symptoms that might suggest the disease is getting worse, such as fatigue, weight loss, increased pain, decreased bowel and bladder function, and weakness
- Complete blood count (CBC) to monitor for anemia
- Bladder exams every 3 to 6 months after treatment
- Urinalysis if you did not have your bladder removed
How well a person with bladder cancer does depends on the initial stage and response to treatment of the bladder cancer.
The outlook for stage 0 or I cancers is fairly good. Although the risk for the cancer returning is high, most bladder cancers that return can be surgically removed and cured.
The cure rates for people with stage III tumors are less than 50%. People with stage IV bladder cancer are rarely cured.
Possible Complications
Bladder cancers may spread into the nearby organs. They may also travel through the pelvic lymph nodes and spread to the liver, lungs, and bones. Additional complications of bladder cancer include:
-
Anemia
Anemia
Anemia is a condition in which the body does not have enough healthy red blood cells. Red blood cells provide oxygen to body tissues. Different type...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Swelling of the ureters (
hydronephrosis
)
Hydronephrosis
Hydronephrosis is swelling of one kidney due to a backup of urine. This problem may occur in one kidney.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Urethral stricture
Urethral stricture
Urethral stricture is an abnormal narrowing of the urethra. Urethra is the tube that carries urine out of the body from the bladder.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Urinary incontinence
When to Contact a Medical Professional
Call your health care provider if you have blood in your urine or other symptoms of bladder cancer, including:
- Frequent urination
- Painful urination
- Urgent need to urinate
Prevention
If you smoke, quit. Smoking can increase your risk for bladder cancer. Avoid exposure to chemicals linked to bladder cancer.
References
National Cancer Institute: PDQ bladder cancer treatment. Bethesda, MD: National Cancer Institute. Updated February 18, 2016. www.cancer.gov/cancertopics/pdq/treatment/bladder/healthprofessional . Accessed April 4, 2016.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology (NCCN guidelines): Bladder cancer. Version 2.2015. www.nccn.org/professionals/physician_gls/pdf/bladder.pdf . Accessed April 4, 2016.
Smith A, Balar AV, Milowsky MI, Chen RC. Bladder cancer. In: Niederhuber JE, Armitage JO, Doroshow JH, Kastan MB, Tepper JE, eds. Abeloff's Clinical Oncology . 5th ed. Philadelphia, PA: Elsevier; 2014:chap 83.
-
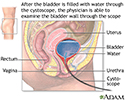
Cystoscopy - illustration
Cystoscopy is a procedure that uses a flexible fiber optic scope inserted through the urethra into the urinary bladder. The physician fills the bladder with water and inspects the interior of the bladder. The image seen through the cystoscope may also be viewed on a color monitor and recorded on videotape for later evaluation.
Cystoscopy
illustration
-
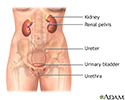
Female urinary tract - illustration
The female and male urinary tracts are relatively the same except for the length of the urethra.
Female urinary tract
illustration
-
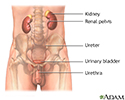
Male urinary tract - illustration
The male and female urinary tracts are relatively the same except for the length of the urethra.
Male urinary tract
illustration
-
Cystoscopy - illustration
Cystoscopy is a procedure that uses a flexible fiber optic scope inserted through the urethra into the urinary bladder. The physician fills the bladder with water and inspects the interior of the bladder. The image seen through the cystoscope may also be viewed on a color monitor and recorded on videotape for later evaluation.
Cystoscopy
illustration
-
Female urinary tract - illustration
The female and male urinary tracts are relatively the same except for the length of the urethra.
Female urinary tract
illustration
-
Male urinary tract - illustration
The male and female urinary tracts are relatively the same except for the length of the urethra.
Male urinary tract
illustration
Review Date: 3/16/2016
Reviewed By: Todd Gersten, MD, Hematology/Oncology, Florida Cancer Specialists & Research Institute, Wellington, FL. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.