Subdural hematoma
Subdural hemorrhage; Traumatic brain injury - subdural hematoma; TBI - subdural hematoma; Head injury - subdural hematoma
A subdural hematoma is a collection of blood between the covering of the brain (dura) and the surface of the brain.
Causes
A subdural hematoma is most often the result of a severe head injury. This type of subdural hematoma is among the deadliest of all head injuries. The bleeding fills the brain area very rapidly, compressing brain tissue. This often results in brain injury and may lead to death.
Subdural hematomas can also occur after a minor head injury. The amount of bleeding is smaller and occurs more slowly. This type of subdural hematoma is often seen in older adults. These may go unnoticed for many days to weeks, and are called chronic subdural hematomas .
Chronic subdural hematomas
A chronic subdural hematoma is an "old" collection of blood and blood breakdown products between the surface of the brain and its outermost covering ...
With any subdural hematoma, tiny veins between the surface of the brain and its outer covering (the dura) stretch and tear, allowing blood to collect. In older adults, the veins are often already stretched because of brain shrinkage (atrophy) and are more easily injured.
Some subdural hematomas occur without cause (spontaneously).
The following increase the risk for a subdural hematoma:
- Medicines that thin the blood (such as warfarin or aspirin)
- Long-term alcohol use
- Medical conditions that make your blood clot poorly
- Repeated head injury, such as from falls
- Very young or very old age
In infants and young children, a subdural hematoma may occur after child abuse.
Symptoms
Depending on the size of the hematoma and where it presses on the brain, any of the following symptoms may occur:
- Confused or slurred speech
- Problems with balance or walking
- Headache
- Lack of energy or confusion
- Seizures or loss of consciousness
- Nausea and vomiting
- Weakness or numbness
- Vision problems
In infants, symptoms may include:
-
Bulging fontanelles
(the soft spots of the baby's skull)
Bulging fontanelles
A bulging fontanelle is an outward curving of an infant's soft spot (fontanelle).
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Separated sutures (the areas where growing skull bones join)
- Feeding problems
-
Seizures
Seizures
A seizure is the physical findings or changes in behavior that occur after an episode of abnormal electrical activity in the brain. The term "seizure...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - High-pitched cry, irritability
- Increased head size (circumference)
- Increased sleepiness or lethargy
- Persistent vomiting
Exams and Tests
Get medical help right away after a head injury. Do not delay. Older adults should receive medical care if they show signs of memory problems or mental decline, even if they don't seem to have an injury.
The health care provider will likely order a brain imaging test, such as a CT or MRI scan , if there are any of the symptoms listed above.
CT
A head computed tomography (CT) scan uses many x-rays to create pictures of the head, including the skull, brain, eye sockets, and sinuses.

MRI scan
A head MRI (magnetic resonance imaging) is an imaging test that uses powerful magnets and radio waves to create pictures of the brain and surrounding...

Treatment
A subdural hematoma is an emergency condition.
Emergency surgery may be needed to reduce pressure within the brain. This may involve drilling a small hole in the skull to drain any blood and relieve pressure on the brain. Large hematomas or solid blood clots may need to be removed through a procedure called a craniotomy , which creates a larger opening in the skull.
Craniotomy
Brain surgery is an operation to treat problems in the brain and surrounding structures.

Medicines that may be used depend on the type of subdural hematoma, how severe the symptoms are, and how much brain damage there is. has occurred. Medicines may include:
- Diuretics (water pills) and corticosteroids to reduce swelling
- Anti-seizure drugs to control or prevent seizures
Outlook (Prognosis)
Outlook depends on the type and location of head injury, the size of the blood collection, and how soon treatment is started.
Acute subdural hematomas have high rates of death and brain injury. Chronic subdural hematomas have better outcomes in most cases. Symptoms often go away after the blood collection is drained. Physical therapy is sometimes needed to help the person get back to their usual level of functioning.
Seizures often occur at the time the hematoma forms, or up to months or years after treatment. But medicines can help control the seizures.
Possible Complications
Complications that may result include:
-
Brain herniation
(pressure on the brain severe enough to cause coma and death)
Brain herniation
A brain herniation is when brain tissue, cerebrospinal fluid, and blood vessels are moved or pressed away from their usual position inside the skull....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Persistent symptoms such as memory loss,
dizziness
,
headache
,
anxiety
, and difficulty concentrating
Dizziness
Dizziness is a term that is often used to describe 2 different symptoms: lightheadedness and vertigo. Lightheadedness is a feeling that you might fai...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleHeadache
A headache is pain or discomfort in the head, scalp, or neck. Serious causes of headaches are rare. Most people with headaches can feel much better...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleAnxiety
Stress is a feeling of emotional or physical tension. It can come from any event or thought that makes you feel frustrated, angry, or nervous. Stres...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Seizures
- Short-term or permanent weakness, numbness, difficulty speaking
When to Contact a Medical Professional
A subdural hematoma is a medical emergency. Call 911 or your local emergency number, or go to an emergency room after a head injury. Do not delay.
Spinal injuries often occur with head injuries, so try to keep the person's neck still if you must move them before help arrives.
Prevention
Always use safety equipment at work and play to reduce your risk of a head injury. For example, use hard hats, bicycle or motorcycle helmets, and seat belts. Older individuals should be particularly careful to avoid falls.
References
Heegaard WG, Biros MH. Head injury. In: Marx JA, Hockberger RS, Walls RM, et al, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice . 8th ed. Philadelphia, PA: Elsevier Saunders; 2014:chap 41.
Stippler M. Craniocerebral trauma. In: Daroff RB, Jankovic J, Mazziotta JC, Pomeroy SL, eds. Bradley's Neurology in Clinical Practice . 7th ed. Philadelphia, PA: Elsevier; 2016:chap 62.
-
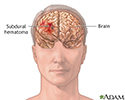
Subdural hematoma - illustration
Subdural hematoma develops when blood veins that are located between the membranes covering the brain (the meninges) leak blood after an injury to the head. This is a serious condition since the increase in intracranial pressure can cause damage to brain tissue and loss of brain function.
Subdural hematoma
illustration
-
Increased intracranial pressure - illustration
Increased intracranial pressure is almost always indicative of severe medical problems. The pressure itself can be responsible for further damage to the central nervous system by decreasing blood flow to the brain or by causing the brain to herniate (push through) the opening in the back of the skull where the spinal cord is attached. Causes of increased intracranial presure may include bleeding into the subdural space (subdural hematoma).
Increased intracranial pressure
illustration
-
Subdural hematoma - illustration
Subdural hematoma develops when blood veins that are located between the membranes covering the brain (the meninges) leak blood after an injury to the head. This is a serious condition since the increase in intracranial pressure can cause damage to brain tissue and loss of brain function.
Subdural hematoma
illustration
-
Increased intracranial pressure - illustration
Increased intracranial pressure is almost always indicative of severe medical problems. The pressure itself can be responsible for further damage to the central nervous system by decreasing blood flow to the brain or by causing the brain to herniate (push through) the opening in the back of the skull where the spinal cord is attached. Causes of increased intracranial presure may include bleeding into the subdural space (subdural hematoma).
Increased intracranial pressure
illustration
Review Date: 5/30/2016
Reviewed By: Amit M. Shelat, DO, FACP, Attending Neurologist and Assistant Professor of Clinical Neurology, SUNY Stony Brook, School of Medicine, Stony Brook, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.