Optic neuritis
Retro-bulbar neuritis; Multiple sclerosis - optic neuritis; Optic nerve - optic neuritis
The optic nerve carries images of what the eye sees to the brain. When this nerve become swollen or inflamed, it is called optic neuritis. It may cause sudden, reduced vision in the affected eye.
Causes
The exact cause of optic neuritis is unknown.
The optic nerve carries visual information from your eye to the brain. The nerve can swell when it becomes suddenly inflamed. The swelling can damage nerve fibers. This can cause short or long-term loss of vision.
Conditions that have been linked with optic neuritis include:
-
Autoimmune diseases
, including
lupus
,
sarcoidosis
, and Behçet disease
Autoimmune diseases
An autoimmune disorder occurs when the body's immune system attacks and destroys healthy body tissue by mistake. There are more than 80 types of aut...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleLupus
Systemic lupus erythematosus (SLE) is an autoimmune disease. In this disease, the body's immune system mistakenly attacks healthy tissue. It can af...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleSarcoidosis
Sarcoidosis is a disease in which inflammation occurs in the lymph nodes, lungs, liver, eyes, skin, or other tissues.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Cryptococcosis
, a fungal infection
Cryptococcosis
Cryptococcosis is infection with the fungi Cryptococcus neoformans and Cryptococcus gattii.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Bacterial infections, including tuberculosis, syphilis,
Lyme disease
, and
meningitis
Lyme disease
Lyme disease is a bacterial infection that is spread through the bite of one of several types of ticks.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleMeningitis
Meningitis is an infection of the membranes covering the brain and spinal cord. This covering is called the meninges.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Viral infections, including viral
encephalitis
,
measles
,
rubella
,
chickenpox
,
herpes zoster
,
mumps
, and mononucleosis
Encephalitis
Encephalitis is irritation and swelling (inflammation) of the brain, most often due to infections.
Read Article Now Book Mark ArticleMeasles
Measles is a very contagious (easily spread) illness caused by a virus.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleRubella
Rubella, also known as the German measles, is an infection in which there is a rash on the skin. Congenital rubella is when a pregnant woman with rub...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleChickenpox
Chickenpox is a viral infection in which a person develops very itchy blisters all over the body. It was more common in the past. The illness is ra...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleHerpes zoster
Shingles (herpes zoster) is a painful, blistering skin rash. It is caused by the varicella-zoster virus. This is the virus that also causes chicken...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleMumps
Mumps is a contagious disease that leads to painful swelling of the salivary glands. The salivary glands produce saliva, a liquid that moistens food...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Respiratory infections, including
mycoplasma pneumonia
and other common upper respiratory tract infections
Mycoplasma pneumonia
Pneumonia is inflamed or swollen lung tissue due to infection with a germ. Mycoplasma pneumonia is caused by the bacteria Mycoplasma pneumoniae (M pn...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Multiple sclerosis
Multiple sclerosis
Multiple sclerosis is an autoimmune disease that affects the brain and spinal cord (central nervous system).
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Symptoms
Symptoms may include:
-
Loss of vision
in 1 eye over an hour or a few hours
Loss of vision
Blindness is a lack of vision. It may also refer to a loss of vision that cannot be corrected with glasses or contact lenses. Partial blindness mean...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Changes in the way the pupil reacts to bright light
- Loss of color vision
- Pain when you move the eye
Exams and Tests
A complete medical exam can help rule out related diseases. Tests may include:
- Color vision testing
-
MRI of the brain
, including special images of the optic nerve
MRI of the brain
A head MRI (magnetic resonance imaging) is an imaging test that uses powerful magnets and radio waves to create pictures of the brain and surrounding...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Visual acuity testing
Visual acuity testing
The visual acuity test is used to determine the smallest letters you can read on a standardized chart (Snellen chart) or a card held 20 feet (6 meter...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Visual field testing
-
Examination of the optic disc using indirect
ophthalmoscopy
Ophthalmoscopy
Ophthalmoscopy is an examination of the back part of the eye (fundus), which includes the retina, optic disc, choroid, and blood vessels.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
Vision often returns to normal within 2 to 3 weeks with no treatment.
Corticosteroids given through a vein (IV) or taken by mouth (oral) may speed up recovery. However, the final vision is no better with steroids than without. Oral steroids may actually increase the chance of recurrence.
Further tests may be needed to find the cause of the neuritis. The condition causing the problem can then be treated.
Outlook (Prognosis)
People who have optic neuritis without a disease such as multiple sclerosis have a good chance of recovery.
Optic neuritis caused by multiple sclerosis or other autoimmune diseases has a poorer outlook. However, vision in the affected eye may still return to normal.
Multiple sclerosis
Multiple sclerosis is an autoimmune disease that affects the brain and spinal cord (central nervous system).

Possible Complications
Complications may include:
- Body-wide side effects from corticosteroids
- Vision loss
Some people who have an episode of optic neuritis will develop nerve problems in other places in the body or develop multiple sclerosis.
When to Contact a Medical Professional
Call your health care provider right away if you have a sudden loss of vision in one eye, especially if you have eye pain.
If you have been diagnosed with optic neuritis, call your health care provider if:
- Your vision decreases.
-
The
pain in the eye
gets worse.
Pain in the eye
Pain in the eye may be described as a burning, throbbing, aching, or stabbing sensation in or around the eye. It may also feel like you have a forei...
Read Article Now Book Mark Article - Your symptoms do not improve within 2 to 3 weeks.
References
Eze P, Sra SK, Sra KK, Friedlaender M, Trocme SD. Immunology of neurologic and endocrine diseases that affect the eye. In: Tasman W, Jaeger EA, eds. Duane's Foundations of Clinical Ophthalmology . 2013 ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2013:vol 2,chap 35.
Jacobs DA, Guercio JR, Balcer LJ. Inflammatory optic neuropathies and neuroretinitis. In: Yanoff M, Duker JS, eds. Ophthalmology . 4th ed. Philadelphia, PA: Elsevier; 2014:chap 9.7.
Prasad S, Balcer LJ. Abnormalities of the optic nerve and retina. In: Daroff RB, Jankovic J, Mazziotta JC, Pomeroy SL, eds. Bradley's Neurology in Clinical Practice . 7th ed. Philadelphia, PA: Elsevier; 2016:chap 17.
Purvin V, Glaser JS. Topical diagnosis: prechiasmal visual pathways. In: Tasman W, Jaeger EA, eds. Duane's Ophthalmology . 2013 ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2013:vol 2,chap 5.
-
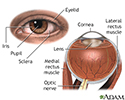
External and internal eye anatomy - illustration
The cornea allows light to enter the eye. As light passes through the eye the iris changes shape by expanding and letting more light through or constricting and letting less light through to change pupil size. The lens then changes shape to allow the accurate focusing of light on the retina. Light excites photoreceptors that eventually, through a chemical process, transmit nerve signals through the optic nerve to the brain. The brain processes these nerve impulses into sight.
External and internal eye anatomy
illustration
-
External and internal eye anatomy - illustration
The cornea allows light to enter the eye. As light passes through the eye the iris changes shape by expanding and letting more light through or constricting and letting less light through to change pupil size. The lens then changes shape to allow the accurate focusing of light on the retina. Light excites photoreceptors that eventually, through a chemical process, transmit nerve signals through the optic nerve to the brain. The brain processes these nerve impulses into sight.
External and internal eye anatomy
illustration
Review Date: 3/15/2016
Reviewed By: Franklin W. Lusby, MD, ophthalmologist, Lusby Vision Institute, La Jolla, CA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.