Chronic inflammatory demyelinating polyneuropathy
Polyneuropathy - chronic inflammatory; CIDP; Chronic inflammatory polyneuropathy; Guillain-Barré - CIDP
Chronic inflammatory demyelinating polyneuropathy (CIDP) is a disorder that involves nerve swelling and irritation (inflammation) that leads to a loss of strength or sensation.
Causes
CIDP is one cause of damage to nerves outside the brain or spinal cord ( peripheral neuropathy ). Polyneuropathy means several nerves are involved. CIDP often affects both sides of the body.
Peripheral neuropathy
Peripheral nerves carry information to and from the brain. They also carry signals to and from the spinal cord to the rest of the body. Peripheral n...

CIDP is caused by an abnormal immune response . CIDP occurs when the immune system attacks the myelin cover of the nerves. For this reason CIDP is thought to be an autoimmune disease .
Immune response
The immune response is how your body recognizes and defends itself against bacteria, viruses, and substances that appear foreign and harmful....

Myelin cover
Myelin is an insulating layer, or sheath that forms around nerves, including those in the brain and spinal cord. It is made up of protein and fatty ...

Autoimmune disease
An autoimmune disorder occurs when the body's immune system attacks and destroys healthy body tissue by mistake. There are more than 80 types of aut...

Health care providers also consider CIDP as the chronic form of Guillain-Barré syndrome.
Chronic
Chronic refers to something that continues over an extended period of time. A chronic condition is usually long-lasting and does not easily or quick...

The specific triggers of CIDP vary. In many cases, the cause cannot be identified.
CIDP may occur with other conditions, such as:
-
Chronic
hepatitis
Hepatitis
Hepatitis is swelling and inflammation of the liver.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Diabetes
- HIV/AIDS
- Immune system disorders due to cancer
-
Inflammatory bowel disease
Inflammatory bowel disease
Ulcerative colitis is a condition in which the lining of the large intestine (colon) and rectum become inflamed. It is a form of inflammatory bowel ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Systemic lupus erythematosus
Systemic lupus erythematosus
Systemic lupus erythematosus (SLE) is an autoimmune disease. In this disease, the body's immune system mistakenly attacks healthy tissue. It can af...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Cancer of the lymph system
- Overactive thyroid
- Side effects of medicines to treat cancer or HIV
Symptoms
Symptoms include any of the following:
-
Problems walking
due to weakness or lack of feeling in the feet
Problems walking
Walking abnormalities are unusual and uncontrollable walking patterns. They are usually due to diseases or injuries to the legs, feet, brain, spinal...
Read Article Now Book Mark Article - Trouble using the arms and hands or legs and feet due to weakness
-
Sensation changes
, such as numbness or decreased sensation, pain, burning, tingling, or other abnormal sensations (usually affects the feet first, then the arms and hands)
Sensation changes
Numbness and tingling are abnormal sensations that can occur anywhere in your body, but they are often felt in your fingers, hands, feet, arms, or le...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Other symptoms that can occur with CIDP include:
- Abnormal or uncoordinated movement
- Problems breathing
-
Fatigue
Fatigue
Fatigue is a feeling of weariness, tiredness, or lack of energy.
Read Article Now Book Mark Article -
Hoarseness or changing voice
or slurred speech
Hoarseness or changing voice
Hoarseness refers to a difficulty making sounds when trying to speak. Vocal sounds may be weak, breathy, scratchy, or husky, and the pitch or qualit...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Exams and Tests
The health care provider will perform a physical exam and ask about the symptoms, focusing on the nervous system and muscles.
Tests that may be ordered include:
-
Electromyography (
EMG
) to check the muscles and the nerves that control the muscles
EMG
Electromyography (EMG) is a test that checks the health of the muscles and the nerves that control the muscles.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Nerve conduction tests
to check how fast electrical signals move through a nerve
Nerve conduction tests
Nerve conduction velocity (NCV) is a test to see how fast electrical signals move through a nerve.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Nerve biopsy
to remove a small piece of a nerve for examination
Nerve biopsy
A nerve biopsy is the removal of a small piece of a nerve for examination.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Spinal tap
(lumbar puncture) to check the fluid that surrounds the brain and spinal cord
Spinal tap
Cerebrospinal fluid (CSF) collection is a test to look at the fluid that surrounds the brain and spinal cord. CSF acts as a cushion, protecting the b...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Blood tests may be done to look for specific proteins that are causing the immune attack on the nerves
Depending on the suspected cause of CIDP, other tests, such as x-rays , imaging scans, and blood tests, may be done.
x-rays
X-rays are a type of electromagnetic radiation, just like visible light. An x-ray machine sends individual x-ray particles through the body. The im...

Treatment
The goal of treatment is to reverse the attack on the nerves. In some cases, nerves can heal and their function can be restored. In other cases, nerves are badly damaged and cannot heal, so treatment is aimed at preventing the disease from getting worse.
Which treatment is given depends on how severe the symptoms are, among other things. The most aggressive treatment is only given if you have difficulty walking or if symptoms don't allow you to care for yourself or work.
Treatments may include:
- Corticosteroids to help reduce inflammation and relieve symptoms
- Other medicines that suppress the immune system (for some severe cases)
-
Plasmapheresis or plasma exchange to remove
antibodies
from the blood
Antibodies
An antibody is a protein produced by the body's immune system when it detects harmful substances, called antigens. Examples of antigens include micr...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Intravenous immune globulin (IVIg), which involves adding large numbers of antibodies to the blood plasma to reduce the effect of the antibodies that are causing the problem
Outlook (Prognosis)
The outcome varies. The disorder may continue long term, or you may have repeated episodes of symptoms. Complete recovery is possible, but permanent loss of nerve function is not uncommon.
Possible Complications
Complications of CIDP include:
- Pain
- Permanent decrease or loss of sensation in areas of the body
- Permanent weakness or paralysis in areas of the body
- Repeated or unnoticed injury to an area of the body
- Side effects of medicines used to treat the disorder
When to Contact a Medical Professional
Call your provider if you have a loss of movement or sensation in any area of the body, especially if your symptoms get worse.
References
Katirji B. Disorders of peripheral nerves. In: Daroff RB, Jankovic J, Mazziotta JC, Pomeroy SL, eds. Bradley's Neurology in Clinical Practice . 7th ed. Philadelphia, PA: Elsevier; 2016:chap 107.
Shy ME. Peripheral neuropathies. In: Goldman L, Schafer AI, eds. Goldman's Cecil Medicine . 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 420.
-
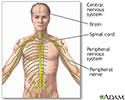
Central nervous system - illustration
The central nervous system is comprised of the brain and spinal cord. The peripheral nervous system includes all peripheral nerves.
Central nervous system
illustration
Review Date: 5/30/2016
Reviewed By: Amit M. Shelat, DO, FACP, Attending Neurologist and Assistant Professor of Clinical Neurology, SUNY Stony Brook, School of Medicine, Stony Brook, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.