Creutzfeldt-Jakob disease
Transmissible spongiform encephalopathy; vCJD; CJD; Jacob-Creutzfeldt disease
Creutzfeldt-Jakob disease (CJD) is a form of brain damage that leads to a rapid decrease of movement and mental function.
Causes
CJD is caused by a protein called a prion. A prion causes normal proteins to fold abnormally. This affects other proteins' ability to function.
Protein
Proteins are the building blocks of life. Every cell in the human body contains protein. The basic structure of protein is a chain of amino acids. ...

CJD is very rare. It occurs in about 1 of every 1 million people.
There are several types of CJD. The classic types are:
- Sporadic CJD makes up most cases. It occurs for no known reason. The average age at which it starts is 65.
- Familial CJD occurs when a person inherits the abnormal prion from a parent (this form of CJD is rare).
- Acquired CJD includes variant CJD (vCJD), the form related to mad cow disease. Iatrogenic CJD is also an acquired form of the disease. Iatrogenic CJD is sometimes passed through a blood product transfusion, transplant, or contaminated surgical instruments.
Variant CJD is caused by eating infected meat. The infection that causes the disease in cows is believed to be the same one that causes vCJD in humans.
Varient CJD causes less than 1% of all CJD cases. It tends to affect younger people. Fewer than 200 people worldwide have had this disease. Almost all cases occurred in England and France.
CJD may be related to several other diseases caused by prions, including:
- Chronic wasting disease (found in deer)
- Kuru (affected mostly women in New Guinea who ate the brains of dead relatives as part of a funeral ritual)
- Scrapie (found in sheep)
- Other very rare inherited human diseases, such as Gerstmann-Straussler-Scheinker disease and fatal familial insomnia
Symptoms
CJD symptoms may include any of the following:
-
Dementia
that gets worse quickly over a few weeks or months
Dementia
Dementia is a loss of brain function that occurs with certain diseases. It affects memory, thinking, language, judgment, and behavior.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Blurred vision (sometimes)
-
Changes in gait
(walking)
Changes in gait
Walking abnormalities are unusual and uncontrollable walking patterns. They are usually due to diseases or injuries to the legs, feet, brain, spinal...
Read Article Now Book Mark Article -
Confusion
, disorientation
Confusion
Confusion is the inability to think as clearly or quickly as you normally do. You may feel disoriented and have difficulty paying attention, remembe...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Hallucinations (seeing things that aren't there)
- Lack of coordination (for example, stumbling and falling)
- Muscle stiffness
-
Muscle twitching
Muscle twitching
Muscle twitches are fine movements of a small area of muscle.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Nervous, jumpy feelings
- Personality changes
-
Sleepiness
Sleepiness
Drowsiness refers to feeling abnormally sleepy during the day. People who are drowsy may fall asleep in inappropriate situations or at inappropriate...
Read Article Now Book Mark Article - Sudden jerky movements or seizures
- Trouble speaking
Exams and Tests
Early in the disease, a nervous system and mental examination will show memory and thinking problems. Later in the disease, a motor system examination (an exam to test muscle reflexes, strength, coordination, and other physical functions) may show:
- Abnormal reflexes or increased normal reflex responses
- Increase in muscle tone
- Muscle twitching and spasms
- Strong startle response
-
Weakness and loss of muscle tissue (
muscle wasting
)
Muscle wasting
Muscle atrophy is the wasting or loss of muscle tissue.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
There is a loss of coordination and changes in the cerebellum. This is the area of the brain that controls coordination. An eye exam shows areas of blindness that the person may not notice.
Tests used to diagnose this condition may include:
- Blood tests to rule out other forms of dementia and to look for markers that sometimes occur with the disease
-
CT scan of the brain
CT scan of the brain
A head computed tomography (CT) scan uses many x-rays to create pictures of the head, including the skull, brain, eye sockets, and sinuses.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Electroencephalogram
(EEG)
Electroencephalogram
An electroencephalogram is a test to measure the electrical activity of the brain.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
MRI of the brain
MRI of the brain
A head MRI (magnetic resonance imaging) is an imaging test that uses powerful magnets and radio waves to create pictures of the brain and surrounding...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Spinal tap
to test for a protein called 14-3-3
Spinal tap
Cerebrospinal fluid (CSF) collection is a test to look at the fluid that surrounds the brain and spinal cord. CSF acts as a cushion, protecting the b...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
The disease can only be confirmed with a brain biopsy or autopsy. Today, it is very rare for a brain biopsy to be done to look for this disease.
Treatment
There is no known cure for this condition. Different medicines have been tried to slow the disease. These include antibiotics, drugs for epilepsy, blood thinners, antidepressants, and interferon. But none works well.
The goal of treatment is to provide a safe environment, control aggressive or agitated behavior, and meet the person's needs. This may require monitoring and assistance in the home or in a care facility. Family counseling may help the family cope with the changes needed for home care.
People with this condition may need help controlling unacceptable or dangerous behaviors. This involves rewarding positive behaviors and ignoring negative behaviors (when it is safe). They may also need help getting oriented to their surroundings. Sometimes, medicines are needed to help control aggression.
Persons with CJD and their family may need to seek legal advice early in the course of the disorder. Advance directive , power of attorney, and other legal actions can make it easier to make decisions about the care of the person with CJD.
Advance directive
Living will; Power of attorney; DNR - advance directive; Do not resuscitate - advance directive; Do-not-resuscitate - advance directive; Durable powe...

Outlook (Prognosis)
The outcome of CJD is very poor. People with sporadic CJD are unable to care for themselves within 6 months or less after symptoms begin.
The disorder is fatal in a short time, usually within 8 months. People who have variant CJD get worse more slowly, but the condition is still fatal. A few people survive for as long as 1 or 2 years. The cause of death is usually infection, heart failure, or respiratory failure.
The course of CJD is:
- Infection with the disease
- Loss of ability to interact with others
- Loss of ability to function or care for oneself
- Death
When to Contact a Medical Professional
CJD is not a medical emergency. However, getting diagnosed and treated early may make the symptoms easier to control, give patients time to make advance directives and prepare for the end of life, and give families extra time to come to terms with the condition.
Prevention
Medical equipment that may be contaminated should be removed from service and disposed of. People known to have CJD should not donate a cornea or other body tissue.
Most countries now have strict guidelines for managing infected cows to avoid transmitting CJD to humans
References
Bosque PJ, Tyler KL. Prions and prion diseases of the central nervous system (transmissible neurodegenerative diseases). In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases . 8th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 181.
Sikorska B, Knight R, Ironside JW, Libersk PP. Creutzfeldt-Jakob disease. Adv Exp Med Biol . 2012;724:76-90.
Swaminathan A, Kedar S. Creutzfeldt-Jakob disease. In: Alvero R, Borkan JM, Ferri FF, et al, eds. Ferri's Clinical Advisor . 1st ed. Philadelphia, PA: Elsevier Saunders; 2014.
-
Creutzfeldt-Jakob disease - illustration
Creutzfeldt-Jakob disease is an organic brain syndrome caused by a protein-like particle called a prion. Loss of brain function resembles Alzheimer's disease, but is very rapid in progression. Complete dementia usually occurs by the sixth month, death follows quickly. There is no known cure.
Creutzfeldt-Jakob disease
illustration
-
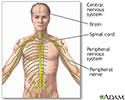
Central nervous system - illustration
The central nervous system is comprised of the brain and spinal cord. The peripheral nervous system includes all peripheral nerves.
Central nervous system
illustration
-
Creutzfeldt-Jakob disease - illustration
Creutzfeldt-Jakob disease is an organic brain syndrome caused by a protein-like particle called a prion. Loss of brain function resembles Alzheimer's disease, but is very rapid in progression. Complete dementia usually occurs by the sixth month, death follows quickly. There is no known cure.
Creutzfeldt-Jakob disease
illustration
-
Central nervous system - illustration
The central nervous system is comprised of the brain and spinal cord. The peripheral nervous system includes all peripheral nerves.
Central nervous system
illustration
Review Date: 8/13/2015
Reviewed By: Joseph V. Campellone, MD, Division of Neurology, Cooper University Hospital, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.