Genital warts
Condylomata acuminata; Penile warts; Human papillomavirus (HPV); Venereal warts; Condyloma; HPV DNA test; Sexually transmitted disease (STD) - warts; Sexually transmitted infection (STI) - warts; LSIL-HPV; Low-grade dysplasia-HPV; HSIL-HPV; High-grade dysplasia HPV; HPV; Cervical cancer - genital warts
Genital warts are soft growths on the skin and mucus membranes of the genitals. They may be found on the penis , vulva , urethra, vagina , cervix , and around and in the anus.
Penis
The penis is the male organ used for urination and sexual intercourse. The penis is located above the scrotum. It is made of spongy tissue and bloo...

Vulva
The vulva is made up of the female genital parts that are outside the body. It includes the "lips" or folds of skin (labia), clitoris, and the openi...

Vagina
The vagina is the female body part that connects the womb (uterus) and cervix to the outside of the body.

Cervix
The cervix is the lower end of the womb (uterus). It is at the top of the vagina. It is about 2 inches (5 centimeters) long. The cervical canal pa...

Genital warts are spread through sexual contact.
Causes
The virus that causes genital warts is called human papillomavirus (HPV). HPV infection is the most common sexually transmitted infection (STI).There are more than 180 types of HPV. Many cause no problems. Some cause warts on other parts of the body and not the genitals. Types 6 and 11 are most commonly linked to genital warts.
Certain other types of HPV can lead to precancerous changes in the cervix , or to cervical cancer . These are called high-risk types of HPV. They can also lead to vaginal or vulvar cancer, anal cancer, and throat or mouth cancer.
Precancerous changes in the cervix
Cervical dysplasia refers to abnormal changes in the cells on the surface of the cervix. The cervix is the lower part of the uterus (womb) that open...

Cervical cancer
Cervical cancer is cancer that starts in the cervix. The cervix is the lower part of the uterus (womb) that opens at the top of the vagina.

Vaginal
Vaginal cancer is cancer of the vagina, a female reproductive organ.

Vulvar
Vulvar cancer is cancer that starts in the vulva. Vulvar cancer most often affects the labia, the folds of skin outside the vagina. In some cases, ...

Throat
Throat cancer is cancer of the vocal cords, larynx (voice box), or other areas of the throat.

Important facts about HPV:
- HPV infection spreads from one person to another through sexual contact involving the anus, mouth, or vagina. The virus can be spread, even if you DO NOT see the warts.
- You may not see warts for 6 weeks to 6 months after becoming infected. You may not notice them for years.
- Not everyone who has come into contact with the HPV virus and genital warts will develop them.
You are more likely to get genital warts and spread them more quickly if you:
- Have multiple sexual partners
- Are sexually active at an early age
- Use tobacco or alcohol
- Have a viral infection, such as herpes, and are stressed at the same time
- Are pregnant
- Have a weakened immune system due to a condition such as diabetes, pregnancy, HIV/AIDS, or from medicines
If a child has genital warts, sexual abuse should be suspected as a possible cause.
Symptoms
Genital warts can be so tiny, you cannot see them.
The warts can look like:
- Flesh-colored spots that are raised or flat
- Growths that look like the top of a cauliflower
In females, genital warts can be found:
- Inside the vagina or anus
- Outside the vagina or anus, or on nearby skin
- On the cervix inside the body
In males, genital warts can be found on the:
- Penis
- Scrotum
- Groin area
- Thighs
- Inside or around the anus
Genital warts can also occur on the
- Lips
- Mouth
- Tongue
- Throat
Other symptoms are rare, but can include:
- Increased dampness in the genital area near the warts
-
Increased vaginal discharge
Increased vaginal discharge
Vaginal discharge refers to secretions from the vagina. The discharge may be:Thick, pasty, or thinClear, cloudy, bloody, white, yellow, or greenOdor...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Genital itching
- Vaginal bleeding during or after sex
Exams and Tests
The health care provider will perform a physical exam. In women, this includes a pelvic exam.
An office procedure called colposcopy is used to spot warts that cannot be seen with the naked eye. It uses a light and a low-power microscope to help your provider find and then take samples ( biopsy ) of abnormal areas in your cervix.
Colposcopy
A colposcopy is a special way of looking at the cervix. It uses a light and a low-powered microscope to make the cervix appear much larger. This he...

Biopsy
A biopsy is the removal of a small piece of tissue for laboratory examination.
The virus that causes genital warts can cause abnormal results on a Pap smear . If you have these types of changes, you may need more frequent Pap smears or a colposcopy.
Pap smear
The Pap test checks for cervical cancer. Cells scraped from the opening of the cervix are examined under a microscope. The cervix is the lower part...

An HPV DNA test can tell if you have a high-risk type of HPV known to cause cervical cancer. This test may be done:
- If you have genital warts
- As a screening test for women over age 30
- In women of any age who have a slightly abnormal Pap test result
Make sure you are screened for cervical, vaginal, vulvar, or anal cancer if you have been diagnosed with genital warts.
Treatment
Genital warts must be treated by a doctor. DO NOT use over-the-counter medicines meant for other kinds of warts.
Treatment may include:
- Medicines applied to the genital warts or injected by your doctor
- Prescription medicine that you apply at home several times a week
The warts may also be removed with minor procedures, including:
-
Freezing (
cryosurgery
)
Cryosurgery
Cervix cryosurgery is a surgical treatment to freeze and destroy abnormal tissue in the cervix.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Burning (
electrocauterization
)
Electrocauterization
Electrocauterization is the process of heating tissue with electricity.
Read Article Now Book Mark Article -
Laser therapy
Laser therapy
Laser therapy is a medical treatment that uses a strong beam of light to cut, burn, or destroy tissue. The term LASER stands for "Light Amplificatio...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Surgery
Surgery
Surgical excision is the removal of tissue using a sharp knife (scalpel) or other cutting instrument.
Read Article Now Book Mark Article
If you have genital warts, all of your sexual partners should be examined by a provider and treated if warts are found. Even if you DO NOT have symptoms, you should be treated. This is to prevent complications and avoid spreading the condition to others.
You will need to return to your provider after treatment to make sure all the warts are gone.
Regular Pap smears are recommended if you are a woman who has had genital warts, or if your partner had them. If you had warts on your cervix, you may need to have Pap smears every 3 to 6 months after the first treatment.
Women with precancerous changes caused by HPV infection may need further treatment.
Precancerous changes
Cervical dysplasia refers to abnormal changes in the cells on the surface of the cervix. The cervix is the lower part of the uterus (womb) that open...

Outlook (Prognosis)
Many sexually active young women become infected with HPV. In many cases, HPV goes away on its own.
Most men who become infected with HPV never develop any symptoms or problems from the infection. They can still pass it on to current and sometimes future sexual partners.
Even after you have been treated for genital warts, you may still infect others.
Possible Complications
Some types of HPV can cause cancer of the cervix and vulva. They are the main cause of cervical cancer.
Genital warts may become numerous and quite large. These will need further treatment.
When to Contact a Medical Professional
Call your provider if:
- A current or past sexual partner has genital warts
- You have visible warts on your external genitals, itching, discharge, or abnormal vaginal bleeding. Keep in mind that genital warts may not appear for months to years after having sexual contact with an infected person.
- You think a young child might have genital warts
Women should begin having Pap smears at age 21.
Prevention
HPV can be passed from person to person even when there are no visible warts or other symptoms. Practicing safer sex can help reduce your risk of getting HPV and cervical cancer:
- Always use male and female condoms. But be aware that condoms cannot fully protect you. This is because the virus or warts can also be on the nearby skin.
- Have only one sexual partner, who you know is infection-free.
- Limit the number of sexual partners you have over time.
- Avoid partners who take part in high-risk sexual activities.
The human papillomavirus (HPV) vaccine protects against infection by certain strains of HPV. Human papillomavirus can cause cervical cancer and geni...
An HPV vaccine is available:
HPV vaccine
The human papillomavirus (HPV) vaccine protects against infection by certain strains of HPV. Human papillomavirus can cause cervical cancer and geni...
- It protects against the HPV types that cause most HPV cancers in women and men. The vaccines DO NOT treat genital warts, they prevent the infection.
- The vaccine can be given to boys and girls 9 to 12 years old. If the vaccine is given at this age, it is a series of 2 shots.
- If the vaccine is given at 15 years or older, it is a series of 3 shots.
Ask your provider whether the HPV vaccine is right for you or child.
References
Berman B, Amini S. Condyloma acuminata. In: Lebwohl MG, Heymann WR, Berth-Jones J, Coulson I, eds. Treatment of Skin Disease: Comprehensive Therapeutic Strategies . 4th ed. Philadelphia, PA: Elsevier Saunders; 2014:chap 46.
Bonnez W. Papillomaviruses. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases, Updated Edition . 8th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 146.
Centers for Disease Control and Prevention. 2015 sexually transmitted diseases treatment guidelines: anogenital warts. Updated June 4, 2015. Centers for Disease Control Web site. www.cdc.gov/std/tg2015/warts.htm . Accessed December 2, 2016.
Centers for Disease Control and Prevention. Press Release: CDC recommends only two HPV shots for younger adolescents. Updated October 20, 2016. Centers for Disease Control Web site. www.cdc.gov/media/releases/2016/p1020-hpv-shots.html . Accessed December 2, 2016.
Committee on Adolescent Health Care of the American College of Obstetricians and Gynecologists; Immunization Expert Work Group of the American College of Obstetricians and Gynecologists. Committee opinion No. 588: human papillomavirus vaccination. Obstet Gynecol . 2014;123(3):712-718. PMID: 24553168 www.ncbi.nlm.nih.gov/pubmed/24553168 .
-
Cervical cancer
Animation
-
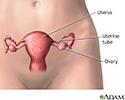
Female reproductive anatomy - illustration
The female reproductive organs are located in the lower abdomen.
Female reproductive anatomy
illustration
Review Date: 8/7/2016
Reviewed By: John D. Jacobson, MD, Professor of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda Center for Fertility, Loma Linda, CA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.