Croup
Viral croup; Laryngotracheobronchitis - acute; Spasmodic croup; Barking cough - croup
Croup is breathing difficulty and a "barking" cough. Croup is due to swelling around the vocal cords. It is common in infants and children.
Breathing difficulty
Breathing difficulty may involve:Difficult breathingUncomfortable breathingFeeling like you are not getting enough air

Causes
Croup is most often caused by viruses such as parainfluenza RSV, measles, adenovirus, and influenza. It tends to appear in children between 3 months and 5 years old, but it can happen at any age. Some children are more likely to get croup and may get it several times. It is most common between October and March, but can occur at any time of the year.
More severe cases of croup may be caused by bacteria. This condition is called bacterial tracheitis.
Croup may also be caused by:
- Allergies
- Breathing in something that irritates your airway
- Acid reflux
Symptoms
The main symptom of croup is a cough that sounds like a seal barking.
Most children will have mild cold symptoms for several days before the barking cough becomes evident. As the cough gets more frequent, the child may have trouble breathing or stridor (a harsh, crowing noise made when breathing in).
Croup is typically much worse at night. It often lasts 5 or 6 nights. The first night or two are most often the worst. Rarely, croup can last for weeks. Talk to your child's health care provider if croup lasts longer than a week or comes back often.
Exams and Tests
Children with croup are most often diagnosed based on the parent's description of the symptoms and a physical exam. Sometimes a provider will listen to a child cough over the phone to identify croup. In a few cases, x-rays or other tests may be needed.
A physical exam may show chest retractions with breathing. When listening to the child's chest through a stethoscope, the health care provider may hear:
- Difficulty breathing in and out
-
Wheezing
Wheezing
Wheezing is a high-pitched whistling sound during breathing. It occurs when air moves through narrowed breathing tubes in the lungs.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Decreased breath sounds
An exam of the throat may reveal a red epiglottis. A neck x-ray may reveal a foreign object or narrowing of the trachea.
Neck x-ray
A neck x-ray is an imaging test to look at cervical vertebrae. These are the 7 bones of the spine in the neck.

Treatment
Most cases of croup can be safely managed at home. However, you should call your provider for advice, even in the middle of the night.
Steps you can take at home include:
- Expose your child to cool or moist air, such as in a steamy bathroom or outside in the cool night air. This may offer some breathing relief.
- Set up a cool air vaporizer in the child's bedroom and use it for a few nights.
- Make your child more comfortable by giving acetaminophen. This medicine also lowers a fever so the child will not have to breathe as hard.
- Avoid cough medicines unless you discuss them with your provider first.
Your provider may prescribe medicines, such as:
- Steroid medicines taken by mouth or through an inhaler
- Antibiotic medicine (for some, but not most cases)
Your child may need to be treated in the emergency room or to stay in the hospital if they:
- Have breathing problems that do not go away or get worse
- Become too tired because of problems breathing
-
Have bluish skin color
Have bluish skin color
Cyanosis is a bluish color to the skin or mucous membrane that is usually due to a lack of oxygen in the blood.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Is not drinking enough fluids
Medicines and treatments used at the hospital may include:
- Breathing medicines given with a nebulizer machine
- Steroid medicines given through a vein (IV)
- An oxygen tent placed over a crib
-
Fluids given through a vein for
dehydration
Dehydration
Dehydration occurs when your body does not have as much water and fluids as it should. Dehydration can be mild, moderate, or severe, based on how muc...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Antibiotics given through a vein
Rarely, a breathing tube through the nose or mouth will be needed to help your child breathe.
Outlook (Prognosis)
Croup is most often mild, but it can still be dangerous. It most often goes away in 3 to 7 days.
The tissue that covers the trachea (windpipe) is called the epiglottis. If the epiglottis becomes infected, the entire windpipe can swell shut. This is a life-threatening condition.
If an airway blockage is not treated promptly, the child can have severe trouble breathing or breathing may stop completely.
Airway blockage
Breathing difficulty may involve:Difficult breathingUncomfortable breathingFeeling like you are not getting enough air

When to Contact a Medical Professional
Most croup can be safely managed at home with telephone support from your provider. Call your provider if your child is not responding to home treatment or is acting more irritable.
Call 911 if:
- Croup symptoms may have been caused by an insect sting or inhaled object.
- Your child has bluish lips or skin color.
- Your child is drooling.
- Your child is having trouble swallowing.
- There is stridor (a noise when breathing in).
- There is a tugging-in of the muscles between the ribs when breathing in.
- Your child is struggling to breathe.
Prevention
Wash your hands frequently and avoid close contact with people who have a respiratory infection.
Many cases of croup can be prevented with immunizations. The diphtheria, Haemophilus influenzae (Hib), and measles vaccines protect children from some of the most dangerous forms of croup.
References
Bower J, McBride JT. Croup in children (acute laryngotracheobronchitis). In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases . 8th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 61.
Cukor J, Manno M. Pediatric respiratory emergencies. In: Marx JA, Hockberger RS, Walls RM, et al, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice . 8th ed. Philadelphia, PA: Elsevier Saunders; 2014:chap 168.
Roosevelt, GE. Acute inflammatory upper airway obstruction (croup, epiglottitis, laryngitis, and bacterial tracheitis). In: Kliegman RM, Stanton BF, St Geme JW, Schor NF, eds. Nelson Textbook of Pediatrics . 20th ed. Philadelphia, PA: Elsevier; 2016:chap 385.
-
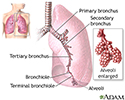
Lungs - illustration
The major features of the lungs include the bronchi, the bronchioles and the alveoli. The alveoli are the microscopic blood vessel-lined sacks in which oxygen and carbon dioxide gas are exchanged.
Lungs
illustration
-
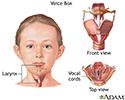
Throat anatomy - illustration
Structures of the throat include the esophagus, trachea, epiglottis and tonsils.
Throat anatomy
illustration
-
Voice box - illustration
The larynx, or voice box, is located in the neck and performs several important functions in the body. The larynx is involved in swallowing, breathing, and voice production. Sound is produced when the air which passes through the vocal cords causes them to vibrate and create sound waves in the pharynx, nose and mouth. The pitch of sound is determined by the amount of tension on the vocal folds.
Voice box
illustration
-
Lungs - illustration
The major features of the lungs include the bronchi, the bronchioles and the alveoli. The alveoli are the microscopic blood vessel-lined sacks in which oxygen and carbon dioxide gas are exchanged.
Lungs
illustration
-
Throat anatomy - illustration
Structures of the throat include the esophagus, trachea, epiglottis and tonsils.
Throat anatomy
illustration
-
Voice box - illustration
The larynx, or voice box, is located in the neck and performs several important functions in the body. The larynx is involved in swallowing, breathing, and voice production. Sound is produced when the air which passes through the vocal cords causes them to vibrate and create sound waves in the pharynx, nose and mouth. The pitch of sound is determined by the amount of tension on the vocal folds.
Voice box
illustration
Review Date: 2/15/2016
Reviewed By: Neil K. Kaneshiro, MD, MHA, Clinical Assistant Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.