Testicular cancer
Cancer - testes; Germ cell tumor; Seminoma testicular cancer; Nonseminoma testicular cancer; Testicular neoplasm
Testicular cancer is cancer that starts in the testicles. The testicles are the male reproductive glands located in the scrotum.
Causes
The exact cause of testicular cancer is unknown. Factors that may increase a man's risk of developing testicular cancer are:
- Abnormal testicle development
- Exposure to certain chemicals
- Family history of testicular cancer
-
HIV infection
HIV infection
Asymptomatic HIV infection is a phase of HIV/AIDS during which there are no symptoms of HIV infection. During this phase, the immune system in someo...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - History of testicular cancer
-
History of an
undescended testicle
(one or both testicles fail to move into the scrotum before birth)
Undescended testicle
Undescended testicle occurs when one or both testicles fail to move into the scrotum before birth.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Klinefelter syndrome
Klinefelter syndrome
Klinefelter syndrome is a genetic condition that occurs in males when they have an extra X chromosome.
Read Article Now Book Mark Article
Testicular cancer is the most common cancer in young and middle-aged men. It can also occur in older men, and in rare cases, in younger boys.
White men are more likely than African American and Asian American men to develop this type of cancer.
There is no link between vasectomy and testicular cancer.
There are two main types of testicular cancer:
- Seminomas
- Nonseminomas
These cancers grow from germ cells, the cells that make sperm.
Seminoma: This is a slow-growing form of testicular cancer found in men in their 30s and 40s. The cancer is in the testes, but it can spread to the lymph nodes. Seminomas are very sensitive to radiation therapy.
Nonseminoma: This more common type of testicular cancer tends to grow more quickly than seminomas.
Nonseminoma tumors are often made up of more than one type of cell, and are identified according to these different cell types:
- Choriocarcinoma (rare)
- Embryonal carcinoma
-
Teratoma
Teratoma
A teratoma is a type of cancer that contains one or more of the three layers of cells found in a developing baby (embryo). These cells are called ge...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Yolk sac tumor
A stromal tumor is a rare type of testicular tumor. They are usually not cancerous. The two main types of stromal tumors are Leydig cell tumors and Sertoli cell tumors. Stromal tumors usually occur during childhood.
Symptoms
There may be no symptoms. The cancer may look like a painless mass in the testes. If there are symptoms, they may include:
- Discomfort or pain in the testicle, or a feeling of heaviness in the scrotum
- Pain in the back or lower abdomen
- Enlarged testicle or a change in the way it feels
-
Excess amount of breast tissue (
gynecomastia
), however this can occur normally in adolescent boys who do not have testicular cancer
Gynecomastia
When abnormally large breasts develop in males, it is called gynecomastia. It is due to the excess growth of breast tissue, not excess fat tissue....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Lump or swelling in either testicle
Symptoms in other parts of the body, such as the lungs, abdomen, pelvis, back, or brain, may also occur if the cancer has spread outside the testicles.
Exams and Tests
A physical examination typically reveals a firm lump (mass) in one of the testicles. When the health care provider holds a flashlight up to the scrotum, the light does not pass through the lump. This exam is called transillumination .
Transillumination
Transillumination is the shining of a light through a body area or organ to check for abnormalities.

Other tests include:
-
Abdominal and pelvic CT scan
Abdominal and pelvic CT scan
An abdominal CT scan is an imaging method. This test uses x-rays to create cross-sectional pictures of the belly area. CT stands for computed tomog...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Blood tests for tumor markers: alpha fetoprotein (AFP), human chorionic gonadotrophin (beta HCG), and lactic dehydrogenase (LDH)
-
Chest x-ray
Chest x-ray
A chest x-ray is an x-ray of the chest, lungs, heart, large arteries, ribs, and diaphragm.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Ultrasound of the scrotum
Ultrasound of the scrotum
Scrotal ultrasound is an imaging test that looks at the scrotum. It is the flesh-covered sac that hangs between the legs at the base of the penis an...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
Treatment depends on the:
- Type of testicular tumor
- Stage of the tumor
Once cancer is found, the first step is to determine the type of cancer cell by examining it under a microscope. The cells can be seminoma, nonseminoma, or both.
The next step is to determine how far the cancer has spread to other parts of the body. This is called "staging."
- Stage I cancer has not spread beyond the testicle.
- Stage II cancer has spread to lymph nodes in the abdomen.
- Stage III cancer has spread beyond the lymph nodes (it could be as far as the liver, lungs, or brain).
Three types of treatment can be used.
- Surgical treatment removes the testicle (orchiectomy).
-
Radiation therapy
using high-dose x-rays or other high-energy rays may be used after surgery to prevent the tumor from returning. Radiation therapy is usually only used for treating seminomas.
Radiation therapy
Radiation therapy uses high-powered x-rays, particles, or radioactive seeds to kill cancer cells.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Chemotherapy
uses drugs to kill cancer cells. This treatment has greatly improved survival for people with both seminomas and nonseminomas.
Chemotherapy
The term chemotherapy is used to describe cancer-killing drugs. Chemotherapy may be used to:Cure the cancerShrink the cancerPrevent the cancer from ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Support Groups
Joining a support group where members share common experiences and problems can often help the stress of illness.
Support group
The following organizations are good resources for information on cancer:American Cancer Society -- www. cancer. orgCancerCare -- www. cancercare. or...
Outlook (Prognosis)
Testicular cancer is one of the most treatable and curable cancers.
The survival rate for men with early-stage seminoma (the least aggressive type of testicular cancer) is greater than 95%. The disease-free survival rate for Stage II and III cancers is slightly lower, depending on the size of the tumor and when treatment is begun.
Possible Complications
Testicular cancer may spread to other parts of the body. The most common sites include the:
- Abdomen
- Lungs
- Retroperitoneal area (the area near the kidneys behind the other organs in the belly area)
- Spine
Complications of surgery can include:
- Bleeding and infection after surgery
- Infertility (if both testicles are removed)
If you think you may want to have children in the future, ask your provider about methods to save your sperm for use at a later date.
When to Contact a Medical Professional
Call your provider if you have symptoms of testicular cancer.
Prevention
Performing a testicular self-examination (TSE) each month may help detect testicular cancer at an early stage, before it spreads. Finding testicular cancer early is important for successful treatment and survival.
Testicular self-examination (TSE)
Testicular self-exam is an examination of the testicles that you do on yourself.

References
Friedlander TW, Ryan CJ, Small EJ, Torti F. Testicular cancer. In: Niederhuber JE, Armitage JO, Doroshow JH, Kastan MB, Tepper JE, eds. Abeloff's Clinical Oncology . 5th ed. Philadelphia, PA: Elsevier Saunders; 2014:chap 86.
National Cancer Institute. PDQ testicular cancer treatment. Updated February 17, 2016. www.cancer.gov/types/testicular/hp/testicular-treatment-pdq#section/_85 . Accessed July 11, 2016.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology (NCCN guidelines): testicular cancer. Version 2.2016. www.nccn.org/professionals/physician_gls/pdf/testicular.pdf . Accessed July 11, 2016.
-
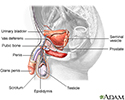
Male reproductive anatomy - illustration
The male reproductive structures include the penis, the scrotum, the seminal vesicles and the prostate.
Male reproductive anatomy
illustration
-
Male reproductive system - illustration
The male reproductive system, viewed from a sagittal section.
Male reproductive system
illustration
-
Male reproductive anatomy - illustration
The male reproductive structures include the penis, the scrotum, the seminal vesicles and the prostate.
Male reproductive anatomy
illustration
-
Male reproductive system - illustration
The male reproductive system, viewed from a sagittal section.
Male reproductive system
illustration
Review Date: 5/20/2016
Reviewed By: Todd Gersten, MD, Hematology/Oncology, Florida Cancer Specialists & Research Institute, Wellington, FL. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.