Lyme disease
Borreliosis; Bannwarth syndrome
Lyme disease is a bacterial infection that is spread through the bite of one of several types of ticks.
Causes
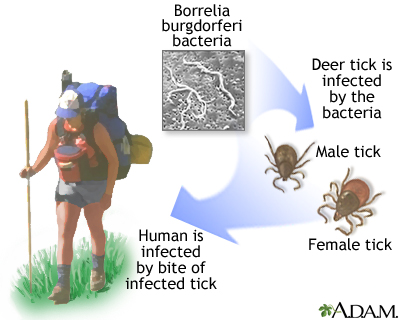
Lyme disease is caused by bacteria called Borrelia burgdorferi ( B burgdorferi ). Blacklegged ticks and other species of ticks can carry these bacteria. The ticks pick up the bacteria when they bite mice or deer that are infected with B burgdorferi . You can get the disease if you are bitten by an infected tick.
Lyme disease was first reported in the United States in 1977 in the town of Old Lyme, Connecticut. The same disease occurs in many parts of Europe and Asia. In the United States, most Lyme disease infections occur in the following areas:
- Northeastern states, from Virginia to Maine
- North-central states, mostly in Wisconsin and Minnesota
- West Coast, mainly in the northwest
There are three stages of Lyme disease.
- Stage 1 is called early localized Lyme disease. The bacteria have not yet spread throughout the body.
- Stage 2 is called early disseminated Lyme disease. The bacteria have begun to spread throughout the body.
- Stage 3 is called late disseminated Lyme disease. The bacteria have spread throughout the body.
Risk factors for Lyme disease include:
- Doing outside activities that increase tick exposure (for example, gardening, hunting, or hiking) in an area where Lyme disease occurs
- Having a pet that may carry infected ticks home
- Walking in high grasses
Important facts about tick bites and Lyme disease:
- A tick must be attached to your body for 24 to 36 hours to spread the bacteria to your blood.
- Blacklegged ticks can be so small that they are almost impossible to see. Many people with Lyme disease never even see or feel a tick on their body.
- Most people who are bitten by a tick do not get Lyme disease.
Symptoms
Symptoms of early localized Lyme disease (stage 1) begin days or weeks after infection. They are similar to the flu and may include:
-
Fever
and chills
Fever
Fever is the temporary increase in the body's temperature in response to a disease or illness. A child has a fever when the temperature is at or abov...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - General ill feeling
-
Headache
Headache
A headache is pain or discomfort in the head, scalp, or neck. Serious causes of headaches are rare. Most people with headaches can feel much better...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Joint pain
-
Muscle pain
Muscle pain
Muscle aches and pains are common and can involve more than 1 muscle. Muscle pain also can involve ligaments, tendons, and fascia. Fascia are the s...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Stiff neck
There may be a "bull's eye" rash, a flat or slightly raised red spot at the site of the tick bite. Often there is a clear area in the center. It can be large and expanding in size. This rash is called erythema migrans. Without treatment, it can last 4 weeks or longer.
Symptoms may come and go. Untreated, the bacteria can spread to the brain, heart, and joints.
Symptoms of early disseminated Lyme disease (stage 2) may occur weeks to months after the tick bite, and may include:
- Numbness or pain in the nerve area
- Paralysis or weakness in the muscles of the face
- Heart problems, such as skipped heartbeats (palpitations), chest pain, or shortness of breath
Symptoms of late disseminated Lyme disease (stage 3) can occur months or years after the infection. The most common symptoms are muscle and joint pain. Other symptoms may include:
- Abnormal muscle movement
- Joint swelling
- Muscle weakness
- Numbness and tingling
- Speech problems
- Thinking (cognitive) problems
Exams and Tests
A blood test can be done to check for antibodies to the bacteria that cause Lyme disease. The most commonly used is the ELISA for Lyme disease test. An immunoblot test is done to confirm ELISA results. Be aware, though, in the early stage of infection, blood tests may be normal. Also, if you are treated with antibiotics in the early stage, your body may not make enough antibodies to be detected by blood tests.
Antibodies
An antibody is a protein produced by the body's immune system when it detects harmful substances, called antigens. Examples of antigens include micr...

ELISA for Lyme disease
The Lyme disease blood test looks for antibodies in the blood to the bacteria that causes Lyme disease. The test is used to help diagnose Lyme disea...

In areas where Lyme disease is more common, your health care provider may be able to diagnose early disseminated Lyme disease (Stage 2) without doing any lab tests.
Other tests that may be done when the infection has spread include:
-
Electrocardiogram
Electrocardiogram
An electrocardiogram (ECG) is a test that records the electrical activity of the heart.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Echocardiogram
to look at the heart
Echocardiogram
An echocardiogram is a test that uses sound waves to create pictures of the heart. The picture and information it produces is more detailed than a s...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
MRI of the brain
MRI of the brain
A head MRI (magnetic resonance imaging) is an imaging test that uses powerful magnets and radio waves to create pictures of the brain and surrounding...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Spinal tap
(lumbar puncture to examine spinal fluid)
Spinal tap
Cerebrospinal fluid (CSF) collection is a test to look at the fluid that surrounds the brain and spinal cord. CSF acts as a cushion, protecting the b...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
People bitten by a tick should be watched closely for at least 30 days to see if a rash or symptoms develop.
A single dose of the antibiotic doxycycline may be given to someone soon after being bitten by a tick, when all of these conditions are true:
- The person has a tick that can carry Lyme disease attached to his or her body. This usually means that a nurse or doctor has looked at and identified the tick.
- The tick is thought to have been attached to the person for at least 36 hours.
- The person is able to start taking the antibiotic within 72 hours of removing the tick.
- The person is 8 years or older and is not pregnant or breastfeeding.
- Local rate of ticks carrying B burgdorferi is 20% or higher.
A 10 day to 4-week course of antibiotics is used to treat people who are diagnosed with Lyme disease, depending on the choice of drug:
- The choice of antibiotic depends on the stage of the disease and the symptoms.
- Common choices include doxycycline, amoxicillin, azithromycin, cefuroxime, and ceftriaxone.
Pain medicines, such as ibuprofen, are sometimes prescribed for joint stiffness .
Outlook (Prognosis)
If diagnosed in the early stages, Lyme disease can be cured with antibiotics. Without treatment, complications involving the joints, heart, and nervous system can occur. But these symptoms are still treatable and curable.
In rare cases, a person keeps having symptoms that interfere with daily life after they have been treated with antibiotics. This is also known as post-Lyme disease syndrome. The cause of this syndrome is unknown.
Symptoms that occur after antibiotics are stopped may not be signs of active infection and may not respond to antibiotic treatment.
Possible Complications
Stage 3, or late disseminated, Lyme disease can cause long-term joint inflammation (Lyme arthritis) and heart rhythm problems. Brain and nervous system problems are also possible, and may include:
- Decreased concentration
- Memory disorders
- Nerve damage
- Numbness
- Pain
- Paralysis of the face muscles
- Sleep disorders
- Vision problems
When to Contact a Medical Professional
Call your provider if you have:
- A large, red, expanding rash that may look like a bull's eye.
- Had a tick bite and develop weakness, numbness, tingling, or heart problems.
- Symptoms of Lyme disease, especially if you may have been exposed to ticks.
Prevention
Take precautions to avoid tick bites. Be extra careful during warmer months. When possible, avoid walking or hiking in the woods and areas with high grass.
If you do walk or hike in these areas, take measures to prevent tick bites:
- Wear light-colored clothing so that if ticks land on you, they can be spotted and removed.
- Wear long sleeves and long pants with pant legs tucked into your socks.
-
Spray exposed skin and your clothing with
insect repellant
, such as DEET or permethrin. Follow instructions on the container.
Insect repellant
The safest bug repellent is to wear proper clothing. Wear a full-brimmed hat to protect your head and the back of your neck. Make sure your ankles an...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - After returning home, remove your clothes and thoroughly inspect all skin surface areas, including your scalp. Shower as soon as possible to wash off any unseen ticks.
If a tick is attached to you, follow these steps to remove it :
Remove it
Ticks are small, insect-like creatures that live in woods and fields. They attach to you as you brush past bushes, plants, and grass. Once on you, ...

- Grasp the tick close to its head or mouth with tweezers. DO NOT use your bare fingers. If needed, use a tissue or paper towel.
- Pull it straight out with a slow and steady motion. Avoid squeezing or crushing the tick. Be careful not to leave the head embedded in the skin.
- Clean the area thoroughly with soap and water. Also wash your hands thoroughly.
- Save the tick in a jar.
- Watch carefully for the next week or two for signs of Lyme disease.
- If all parts of the tick cannot be removed, get medical help. Bring the tick in the jar to your doctor.
References
Centers for Disease Control. Lyme disease. Updated August 19, 2016. www.cdc.gov/lyme . Accessed August 31, 2016.
Steere AC. Lyme disease (Lyme borreliosis) due to Borrelia burgdorferi. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases . 8th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 243.
Wright WF, Riedel DJ, Talwani R, Gilliam BL. Diagnosis and management of Lyme disease. Am Fam Physician . 2012;85(11):1086-1093. PMID: 22962880 www.ncbi.nlm.nih.gov/pubmed/22962880 .
-
Lyme disease organism, Borrelia burgdorferi - illustration
Borrelia burgdorferi is a spirochete bacteria that causes Lyme disease. It is similar in shape to the spirochetes that cause other diseases, such as relapsing fever and syphilis. (Image courtesy of the Centers for Disease Control and Prevention.) Borrelia burgdorferi
Lyme disease organism, Borrelia burgdorferi
illustration
-
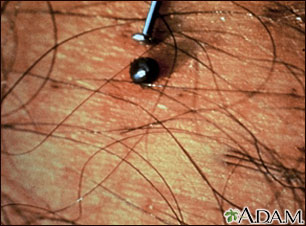
Tick, deer engorged on the skin - illustration
Ixodes dammini
Tick, deer engorged on the skin
illustration
-
Lyme disease - Borrelia burgdorferi organism - illustration
Borrelia burgdorferi.
Lyme disease - Borrelia burgdorferi organism
illustration
-
Tick, deer - adult female - illustration
Ixodes dammini
Tick, deer - adult female
illustration
-
Lyme disease - illustration
Lyme disease is an acute inflammatory disease characterized by skin changes, joint inflammation and symptoms similar to the flu that is caused by the bacterium Borrelia burgdorferi. Lyme disease is transmitted by the bite of a deer tick. Symptoms resolve in 3 to 4 weeks even without treatment, but secondary or tertiary disease may develop if initial infection is not treated. Borrelia burgdorferi
Lyme disease
illustration
-
Lyme disease, erythema migrans - illustration
Erythema migrans is the initial lesion of Lyme disease, and often appears at the site of the infecting tick bite. It is a red, enlarging rash, flat or slightly raised, and may reach from 4 to 20 inches (12 to 35 cm) across (the average rash is 6 inches, or 17 cm). (Image courtesy of the Centers for Disease Control and Prevention.)
Lyme disease, erythema migrans
illustration
-
Tertiary Lyme disease - illustration
Tertiary Lyme disease is a late, persistent inflammatory disease characterized by skin changes, neurological and musculoskeletal symptoms caused by the bacterium Borrelia burgdorferi transmitted by the bite of a tick. Tertiary Lyme disease is indicated by chronic arthritis. Borrelia burgdorferi
Tertiary Lyme disease
illustration
-
Lyme disease organism, Borrelia burgdorferi - illustration
Borrelia burgdorferi is a spirochete bacteria that causes Lyme disease. It is similar in shape to the spirochetes that cause other diseases, such as relapsing fever and syphilis. (Image courtesy of the Centers for Disease Control and Prevention.) Borrelia burgdorferi
Lyme disease organism, Borrelia burgdorferi
illustration
-
Tick, deer engorged on the skin - illustration
Ixodes dammini
Tick, deer engorged on the skin
illustration
-
Lyme disease - Borrelia burgdorferi organism - illustration
Borrelia burgdorferi.
Lyme disease - Borrelia burgdorferi organism
illustration
-
Tick, deer - adult female - illustration
Ixodes dammini
Tick, deer - adult female
illustration
-
Lyme disease - illustration
Lyme disease is an acute inflammatory disease characterized by skin changes, joint inflammation and symptoms similar to the flu that is caused by the bacterium Borrelia burgdorferi. Lyme disease is transmitted by the bite of a deer tick. Symptoms resolve in 3 to 4 weeks even without treatment, but secondary or tertiary disease may develop if initial infection is not treated. Borrelia burgdorferi
Lyme disease
illustration
-
Lyme disease, erythema migrans - illustration
Erythema migrans is the initial lesion of Lyme disease, and often appears at the site of the infecting tick bite. It is a red, enlarging rash, flat or slightly raised, and may reach from 4 to 20 inches (12 to 35 cm) across (the average rash is 6 inches, or 17 cm). (Image courtesy of the Centers for Disease Control and Prevention.)
Lyme disease, erythema migrans
illustration
-
Tertiary Lyme disease - illustration
Tertiary Lyme disease is a late, persistent inflammatory disease characterized by skin changes, neurological and musculoskeletal symptoms caused by the bacterium Borrelia burgdorferi transmitted by the bite of a tick. Tertiary Lyme disease is indicated by chronic arthritis. Borrelia burgdorferi
Tertiary Lyme disease
illustration
-
Lyme disease
(Alt. Medicine)
-
Lyme disease and related tick-borne infections
(In-Depth)
Review Date: 5/1/2015
Reviewed By: Jatin M. Vyas, MD, PhD, Assistant Professor in Medicine, Harvard Medical School; Assistant in Medicine, Division of Infectious Disease, Department of Medicine, Massachusetts General Hospital, Boston, MA. Internal review and update on 09/01/2016 by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.