Cardioversion
Abnormal heart rhythms - cardioversion; Bradycardia - cardioversion; Tachycardia - cardioversion; Fibrillation - cardioversion; Arrhythmia - cardioversion; Cardiac arrest - cardioversion; Defibrillator - cardioversion; Pharmacologic cardioversion
Cardioversion is a method to return an abnormal heart rhythm back to normal.
Information
Cardioversion can be done using an electric shock or with drugs.
ELECTRIC CARDIOVERSION
Electric cardioversion is done with a device that gives off an electrical shock to the heart to change the rhythm back to normal. The device is called a defibrillator.
The shock can be delivered from a device outside the body called an external defibrillator. These are found in emergency rooms, ambulances, or some public places such as airports.
- Electrode patches are placed on the chest and back. The patches are connected to the defibrillator. Or, paddles attached to the devices are placed directly onto the chest.
- The defibrillator is activated and an electric shock is delivered to your heart.
- This shock briefly stops all electrical activity of the heart. Then it allows the normal heart rhythm to return.
- Sometimes more than one shock, or a shock with higher energy is needed.
An external defibrillator is used to treat abnormal heart rhythms ( arrhythmia ) that cause collapse and cardiac arrest. Examples are ventricular tachycardia and ventricular fibrillation.
Arrhythmia
An arrhythmia is a disorder of the heart rate (pulse) or heart rhythm. The heart can beat too fast (tachycardia), too slow (bradycardia), or irregul...

These same devices may also be used to treat less dangerous abnormal rhythms, problems such as atrial fibrillation. The defibrillator will be used when the abnormal and medicines cannot controlled them.
- Some people may need to start blood thinners beforehand to prevent small blood clots.
- You will be given medicine to help you relax before the procedure.
- After the procedure, you may be given medicines to prevent blood clots or to help prevent the arrhythmia from coming back.
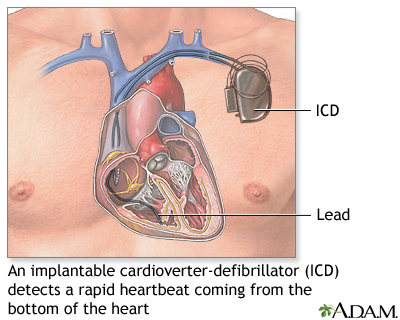
An implantable cardioverter-defibrillator (ICD) is a device that is placed inside your body. It is most often used in people who are at risk for sudden death because there heart function is so poor, or they have had dangerous heart rhythms before.
Implantable cardioverter-defibrillator
An implantable cardioverter-defibrillator (ICD) is a device that detects any life-threatening, rapid heartbeat. This abnormal heartbeat is called an...

- The ICD is implanted underneath the skin of your upper chest or abdomen.
- Wires are attached that go into or near the heart.
- If the device detects a dangerous heartbeat, it sends an electrical shock to the heart to change the rhythm back to normal.
CARDIOVERSION USING DRUGS
Cardioversion can be done using drugs that are taken by mouth or given through an intravenous line (IV). It can take from several minutes to days for this treatment to work. This treatment is often done while in a hospital where your heart rhythm will be monitored.
Cardioversion using drugs can be done outside the hospital. This treatment is most often used for people with atrial fibrillation that comes and goes. However, you will need to be closely followed-up by a cardiologist.
You may be given blood thinning medicines to prevent blood clots from forming and leaving the heart (which can cause a stroke).
COMPLICATIONS
Complications of cardioversion are uncommon, but may include:
- Allergic reactions from medicines used
- Blood clots that can cause a stroke or other organ damage
- Bruising, burning, or pain where the electrodes were used
- Worsening of the arrhythmia
People who perform external cardioversion may be shocked if the procedure is not done correctly. This can cause heart rhythm problems, pain, and even death.
References
Epstein AE, DiMarco JP, Ellenbogen KA, et al. 2012 ACCF/AHA/HRS focused update incorporated into the ACCF/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol . 2013;61(3):e6-e75. PMID: 23265327 www.ncbi.nlm.nih.gov/pubmed/23265327 .
Miller JM, Zipes DP. Therapy for cardiac arrhythmias. In: Bonow RO, Mann DL, Zipes DP, Libby P, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine . 10th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 35.
Myerburg RJ. Approach to cardiac arrest and life-threatening arrhythmias. In: Goldman L, Schafer AI, eds. Goldman's Cecil Medicine . 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 63.
Wilbur DJ. Electrophysiologic interventional procedures and surgery. In: Goldman L, Schafer AI, eds. Goldman's Cecil Medicine . 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 66.
-
Ventricluar fibrillation and tachycardia
Animation
-
Implantable cardioverter-defibrillator - illustration
An implantable cardioverter-defibrillator (ICD) is a device designed to quickly detect a life-threatening, rapid heartbeat coming from the bottom chamber of the heart. It converts the abnormal rhythm back to normal by delivering an electrical shock to the heart.
Implantable cardioverter-defibrillator
illustration
-
Implantable cardioverter-defibrillator - illustration
An implantable cardioverter-defibrillator (ICD) is a device designed to quickly detect a life-threatening, rapid heartbeat coming from the bottom chamber of the heart. It converts the abnormal rhythm back to normal by delivering an electrical shock to the heart.
Implantable cardioverter-defibrillator
illustration
Review Date: 5/5/2016
Reviewed By: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.