Angioplasty and stent placement - peripheral arteries - discharge
Percutaneous transluminal angioplasty - peripheral artery - discharge; PTA - peripheral artery - discharge; Angioplasty - peripheral artery - discharge; Balloon angioplasty - peripheral artery- discharge; PAD - PTA discharge; PVD - PTA discharge
When You're in the Hospital
You had procedure that used a balloon catheter to open a narrowed vessel (angioplasty) that supplies blood to the arms or legs (peripheral artery). You may have also had a stent placed.
To perform the procedure:
- Your doctor inserted a catheter (flexible tube) into your blocked artery through a cut in your groin.
- X-rays were used to guide the catheter up to the area of the blockage.
- The doctor then passed a wire through the catheter to the blockage and a balloon catheter was pushed over it.
- The balloon on the end of the catheter was blown up. This opened the blocked vessel and restored proper blood flow to the affected area.
- A stent is very often placed at the site to prevent the vessel from closing up again.
What to Expect at Home
The cut in your groin may be sore for several days. You should be able to walk farther now without needing to rest, but you should take it easy at first. It may take 6 to 8 weeks to recover fully. Your leg on the side of the procedure may be swollen for a few days or weeks. This will improve as the blood flow to the limb becomes normal.
Self-care
You will need to increase your activity slowly while the incision heals.
- Walking short distances on a flat surface is OK. Try to walk a little bit 3 or 4 times a day. Slowly increase how far you walk each time.
- Limit going up and down stairs to about 2 times a day for the first 2 to 3 days.
- DO NOT do yard work, drive, or play sports for at least 2 days, or for the number of days your health care provider tells you to wait.
You will need to care for your incision.
- Your provider will tell you how often to change your dressing.
- If your incision bleeds or swells up, lie down and put pressure on it for 30 minutes.
- If the bleeding or swelling does not stop or gets worse, call your provider and return to the hospital or else go to the closest emergency room or call 911.
When you are resting, try to keep your legs raised above the level of your heart. Place pillows or blankets under your legs to raise them.
Angioplasty does not cure the cause of blockage in your arteries. Your arteries may become narrow again. To lower your chances of this happening:
-
Eat a
heart-healthy diet
, exercise, stop smoking (if you smoke), and reduce your stress level.
Heart-healthy diet
Hyperlipidemia - cholesterol and lifestyle; CAD - cholesterol and lifestyle; Coronary artery disease - cholesterol and lifestyle; Heart disease - cho...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Take
medicine to help lower your cholesterol
if your provider prescribes it.
Medicine to help lower your cholesterol
Hyperlipidemia - drug treatment; Hardening of the arteries - statin
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - If you are taking medicines for blood pressure or diabetes, take them the way your provider has asked you to take them.
Your provider may recommend that you take aspirin or another medicine, called clopidogrel (Plavix) , when you go home. These medicines keep blood clots from forming in your arteries and in the stent. DO NOT stop taking them without talking with your doctor first.
Aspirin
Blood thinners - aspirin; Antiplatelet therapy - aspirin

Clopidogrel (Plavix)
Blood thinners - clopidogrel; Antiplatelet therapy - clopidogrel; Thienopyridines

When to Call the Doctor
Call your provider if:
- There is swelling at the catheter site.
- There is bleeding at the catheter insertion site that does not stop when pressure is applied.
- Your leg below where the catheter was inserted changes color or becomes cool to the touch, pale, or numb.
- The small incision from your catheter becomes red or painful, or yellow or green discharge is draining from it.
- Your legs are swelling excessively.
- You have chest pain or shortness of breath that does not go away with rest.
- You have dizziness, fainting, or you are very tired.
- You are coughing up blood or yellow or green mucus.
- You have chills or a fever over 101°F (38.3°C).
- You develop weakness in your body, your speech is slurred, or you are unable to get out of bed.
References
Creager MA, Libby P. Peripheral artery diseases. In: Mann DL, Zipes DP, Libby P, Bonow RO, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine . 10th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 58.
Kinlay S, Bhatt D. Treatment of noncoronary obstructive vascular disease. In: Mann DL, Zipes DP, Libby P, Bonow RO, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine . 10th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 60.
-
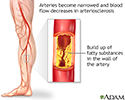
Arteriosclerosis of the extremities - illustration
Atherosclerosis of the extremities is a disease of the peripheral blood vessels that is characterized by narrowing and hardening of the arteries that supply the legs and feet. The narrowing of the arteries causes a decrease in blood flow. Symptoms include leg pain, numbness, cold legs or feet and muscle pain in the thighs, calves or feet.
Arteriosclerosis of the extremities
illustration
-
Arteriosclerosis of the extremities - illustration
Atherosclerosis of the extremities is a disease of the peripheral blood vessels that is characterized by narrowing and hardening of the arteries that supply the legs and feet. The narrowing of the arteries causes a decrease in blood flow. Symptoms include leg pain, numbness, cold legs or feet and muscle pain in the thighs, calves or feet.
Arteriosclerosis of the extremities
illustration
-
Heart attack and acute coronary syndrome
(In-Depth)
Review Date: 5/24/2016
Reviewed By: Mary C. Mancini, MD, PhD, Department of Surgery, Louisiana State University Health Sciences Center-Shreveport, Shreveport, LA. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.