Choking - infant under 1 year
Choking is when someone cannot breathe because food, a toy, or other object is blocking the throat or windpipe (airway).
This article discusses choking in infants.
Causes
Choking in infants is usually caused by breathing in a small object that the baby has placed in their mouth, such as a button, coin, balloon, toy part, or watch battery.
Choking may result from a complete or partial blockage of the airway.
- A complete blockage is a medical emergency.
- A partial blockage can quickly become life-threatening if the baby cannot get enough air.
When a person does not get enough air, permanent brain damage can occur in as little as 4 minutes. Rapid first aid for choking can save a life.
Symptoms
The danger signs of choking are:
- Bluish skin color
- Difficulty breathing - ribs and chest pull inward
- Loss of consciousness if blockage is not cleared
- Inability to cry or make much sound
- Weak, ineffective coughing
- Soft or high-pitched sounds while inhaling
First Aid
Do NOT perform these steps if the infant is coughing hard or has a strong cry. Strong coughs and cries can help push the object out of the airway.
If your child is not coughing forcefully or does not have a strong cry, follow these steps:
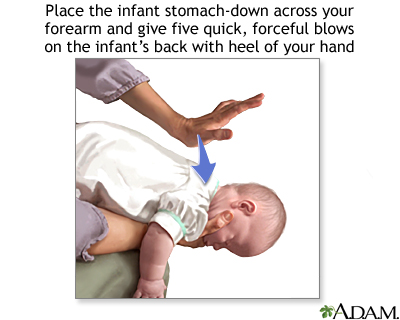
- Lay the infant face down, along your forearm. Use your thigh or lap for support. Hold the infant's chest in your hand and hold the jaw with your fingers. Point the infant's head downward, lower than the body.
- Give up to 5 quick, forceful blows between the infant's shoulder blades. Use the palm of your free hand.
If the object does not come out of the airway after 5 blows:
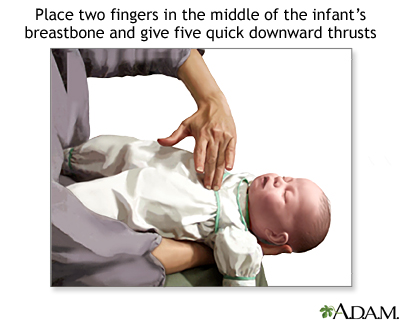
- Turn the infant face-up. Use your thigh or lap for support. Support the head.
- Place 2 fingers on the middle of his breastbone just below the nipples.
- Give up to 5 quick thrusts down, compressing the chest 1/3 to 1/2 the depth of the chest.
- Continue 5 back blows followed by 5 chest thrusts until the object is dislodged or the infant loses alertness (becomes unconscious).
IF THE INFANT LOSES ALERTNESS
If the child becomes unresponsive, stops breathing, or turns blue:
- Shout for help.
-
Give
infant CPR
. Call 911 after 1 minute of CPR.
Infant CPR
CPR stands for cardiopulmonary resuscitation. It is a lifesaving procedure that is done when a baby's breathing or heartbeat has stopped. This may ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - If you can see the object blocking the airway, try to remove it with your finger. Try to remove an object only if you can see it.
Do Not
- Do NOT perform choking first aid if the infant is coughing forcefully, has a strong cry, or is breathing enough. However, be ready to act if the symptoms get worse.
- Do NOT try to grasp and pull out the object if the infant is alert (conscious).
- Do NOT do back blows and chest thrusts if the infant stops breathing for other reasons, such as asthma, infection, swelling, or a blow to the head. Do give infant CPR in these cases.
When to Contact a Medical Professional
If an infant is choking:
- Tell someone to call 911 while you begin first aid.
- If you are alone, shout for help and begin first aid.
Always call your doctor after a child has been choking, even if you successfully remove the object from the airway and the infant seems fine.
Prevention
To prevent choking in an infant:
- Do not give children under 3 years old balloons or toys with small parts that can break off.
- Keep infants away from buttons, popcorn, coins, grapes, nuts, and other small items.
- Watch infants and toddlers while they are eating. Do not allow a child to crawl around while eating.
- The earliest safety lesson is "No!"
References
Berg MD, Schexnayder SM, Chameides L, et al. Part 13: Pediatric basic life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(18 Suppl 3):S862-S875. PMID: 20956229 www.ncbi.nlm.nih.gov/pubmed/20956229 .
Cukor J, Manno M. Pediatric respiratory emergencies. In: Marx J, Hockberger RS, Walls RM, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice. 8th ed. Philadelphia, PA: Elsevier Saunders; 2014:chap 168.
Thomas SH, Goodloe JM. Foreign bodies. In: Marx JA, Hockberger RS, Walls RM, eds.
Rosen's Emergency Medicine: Concepts and Clinical Practice.
8th ed. Philadelphia, PA: Elsevier Saunders; 2014:chap 60.
Review Date: 4/12/2015
Reviewed By: Jacob L. Heller, MD, MHA, Emergency Medicine, Virginia Mason Medical Center, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.