Pulmonary hypertension
Pulmonary arterial hypertension; Sporadic primary pulmonary hypertension; Familial primary pulmonary hypertension; Idiopathic pulmonary arterial hypertension; Primary pulmonary hypertension; PPH; Secondary pulmonary hypertension; Cor pulmonale - pulmonary hypertension
Pulmonary hypertension is high blood pressure in the arteries of the lungs. It makes the right side of the heart work harder than normal.
Causes
The right side of the heart pumps blood through the lungs, where it picks up oxygen. Blood returns to the left side of the heart, where it is pumped to the rest of the body.
When the small arteries (blood vessels) of the lungs become narrowed, they cannot carry as much blood. When this happens, pressure builds up. This is called pulmonary hypertension.
The heart needs to work harder to force the blood through the vessels against this pressure. Over time, this causes the right side of the heart to become larger. This condition is called right-sided heart failure, or cor pulmonale.
Pulmonary hypertension may be caused by:
-
Autoimmune diseases
that damage the lungs, such as
scleroderma
and
rheumatoid arthritis
Autoimmune diseases
An autoimmune disorder occurs when the body's immune system attacks and destroys healthy body tissue by mistake. There are more than 80 types of aut...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleScleroderma
Scleroderma is a disease that involves the buildup of scar-like tissue in the skin and elsewhere in the body. It also damages the cells that line th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleRheumatoid arthritis
Rheumatoid arthritis (RA) is a long-term disease. It leads to inflammation of the joints and surrounding tissues. It can also affect other organs....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Birth defects of the heart
-
Blood clots in the lung (
pulmonary embolism
)
Pulmonary embolism
A pulmonary embolus is a blockage of an artery in the lungs. The most common cause of the blockage is a blood clot.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Heart failure
Heart failure
Heart failure is a condition in which the heart is no longer able to pump oxygen-rich blood to the rest of the body efficiently. This causes symptom...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Heart valve disease
- HIV infection
- Low oxygen levels in the blood for a long time (chronic)
-
Lung disease, such as
COPD
or
pulmonary fibrosis
COPD
Chronic obstructive pulmonary disease (COPD) is a common lung disease. Having COPD makes it hard to breathe. There are two main forms of COPD:Chroni...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticlePulmonary fibrosis
Idiopathic pulmonary fibrosis is scarring or thickening of the lungs without a known cause.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Medicines (for example, certain diet drugs)
-
Obstructive sleep apnea
Obstructive sleep apnea
Obstructive sleep apnea (OSA) is a problem in which your breathing pauses during sleep. This occurs because of narrowed or blocked airways.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
In rare cases, the cause of pulmonary hypertension is unknown. In this case, the condition is called idiopathic pulmonary arterial hypertension (IPAH). Idiopathic means the cause of a disease is not known. IPAH affects more women than men.
If pulmonary hypertension is caused by a known medicine or medical condition, it is called secondary pulmonary hypertension.
Symptoms
Shortness of breath or lightheadedness during activity is often the first symptom. Fast heart rate ( palpitations ) may be present. Over time, symptoms occur with lighter activity or even while at rest.
Palpitations
Palpitations are feelings or sensations that your heart is pounding or racing. They can be felt in your chest, throat, or neck. You may:Have an unpl...

Other symptoms include:
- Ankle and leg swelling
-
Bluish color of the lips or skin (
cyanosis
)
Cyanosis
Cyanosis is a bluish color to the skin or mucous membrane that is usually due to a lack of oxygen in the blood.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Chest pain
or pressure, usually in the front of the chest
Chest pain
Chest pain is discomfort or pain that you feel anywhere along the front of your body between your neck and upper abdomen.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Dizziness
or
fainting
spells
Dizziness
Dizziness is a term that is often used to describe 2 different symptoms: lightheadedness and vertigo. Lightheadedness is a feeling that you might fai...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleFainting
Fainting is a brief loss of consciousness due to a drop in blood flow to the brain. The episode most often lasts less than a couple of minutes and y...
Read Article Now Book Mark Article -
Fatigue
Fatigue
Fatigue is a feeling of weariness, tiredness, or lack of energy.
Read Article Now Book Mark Article - Increased abdomen size
- Weakness
People with pulmonary hypertension often have symptoms that come and go. They report good days and bad days.
Exams and Tests
Your health care provider will perform a physical exam and ask about your symptoms. The exam may find:
- Abnormal heart sounds
- Feeling of a pulse over the breastbone
-
Heart murmur
on the right side of the heart
Heart murmur
A heart murmur is a blowing, whooshing, or rasping sound heard during a heartbeat. The sound is caused by turbulent (rough) blood flow through the h...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Larger-than-normal veins in the neck
- Leg swelling
- Liver and spleen swelling
- Normal breath sounds
In the early stages of the disease, the exam may be normal or almost normal. The condition may take several months to diagnose. Asthma and other diseases may cause similar symptoms and must be ruled out.
Tests that may be ordered include:
- Blood tests
-
Cardiac catheterization
Cardiac catheterization
Cardiac catheterization involves passing a thin flexible tube (catheter) into the right or left side of the heart. The catheter is most often insert...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Chest x-ray
Chest x-ray
A chest x-ray is an x-ray of the chest, lungs, heart, large arteries, ribs, and diaphragm.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
CT scan of the chest
CT scan of the chest
A chest CT (computed tomography) scan is an imaging method that uses x-rays to create cross-sectional pictures of the chest and upper abdomen....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Echocardiogram
Echocardiogram
An echocardiogram is a test that uses sound waves to create pictures of the heart. The picture and information it produces is more detailed than a s...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
ECG
ECG
An electrocardiogram (ECG) is a test that records the electrical activity of the heart.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Lung function tests
-
Nuclear
lung scan
Lung scan
Lung gallium scan is a type of nuclear scan that uses radioactive gallium to identify swelling (inflammation) in the lungs.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Pulmonary arteriogram
Pulmonary arteriogram
Pulmonary angiography is a test to see how blood flows through the lung. Angiography is an imaging test that uses x-rays and a special dye to see in...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - 6-minute walk test
- Sleep study
- Tests to check for autoimmune problems
Treatment
There is no cure for pulmonary hypertension. The goal of treatment is to control symptoms and prevent more lung damage. It is important to treat medical disorders that cause pulmonary hypertension, such as obstructive sleep apnea, lung conditions, and heart valve problems.
Many treatment options for pulmonary arterial hypertension are available. If you are prescribed medicines, they may be taken by mouth (oral), received through the vein (intravenous, or IV), or breathed in (inhaled).
Your provider will decide which medicine is best for you. You will be closely monitored during treatment to watch for side effects and to see how well you are responding to the medicine. DO NOT stop taking your medicines without talking to your provider.
Other treatments may include:
- Blood thinners to reduce the risk of blood clots, especially if you have IPAH
-
Oxygen therapy at home
Oxygen therapy at home
Choking is when someone cannot breathe because food, a toy, or other object is blocking the throat or windpipe (airway). This article discusses cho...
 ImageRead Article Now Book Mark Article
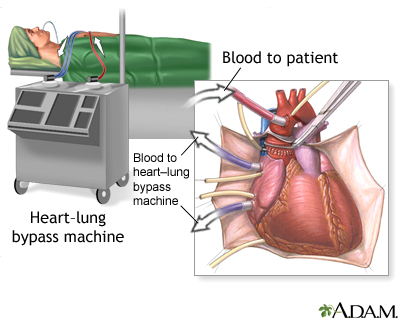
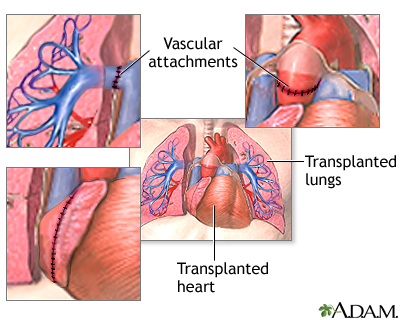
ImageRead Article Now Book Mark Article - Heart-lung transplant, if medicines do not work
Other important tips to follow:
- Avoid pregnancy
- Avoid heavy physical activities and lifting
- Avoid traveling to high altitudes
- Get a yearly flu vaccine, as well as other vaccines such as the pneumonia vaccine
- Stop smoking
Outlook (Prognosis)
How well you do depends on what caused the condition. Medicines for IPAH may help slow the disease.
As the illness gets worse, you will need to make changes in your home to help you get around the house.
Make changes in your home
No definition available for this article.

When to Contact a Medical Professional
Call your provider if:
- You begin to develop shortness of breath when you are active
- Shortness of breath gets worse
- You develop chest pain
- You develop other symptoms
References
Chin K, Channick RN. Pulmonary hypertension. In: Broaddus VC, Mason RJ, Ernst JD, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine . 5th ed. Philadelphia, PA: Elsevier Saunders; 2010:chap 52.
McLaughlin V. Pulmonary hypertension. In: Goldman L, Schafer AI, eds. Goldman's Cecil Medicine . 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 68.
Taichman DB, Ornelas J, Chung L, et al. Pharmacologic therapy for pulmonary arterial hypertension in adults: CHEST guideline and expert panel report. Chest . 2014;146:449-475. PMID: 24937180 www.ncbi.nlm.nih.gov/pubmed/24937180 .
-
Respiratory system - illustration
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Respiratory system
illustration
-
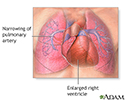
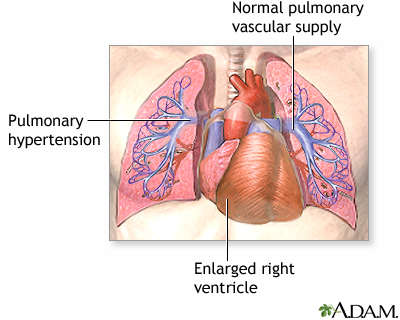
Primary pulmonary hypertension - illustration
Pulmonary hypertension is the narrowing of the pulmonary arterioles within the lung. The narrowing of the arteries creates resistance and an increased work load for the heart. The heart becomes enlarged from pumping blood against the resistance. Some symptoms include chest pain, weakness, shortness of breath, and fatigue. The goal of treatment is control of the symptoms, although the disease usually develops into congestive heart failure.
Primary pulmonary hypertension
illustration
-
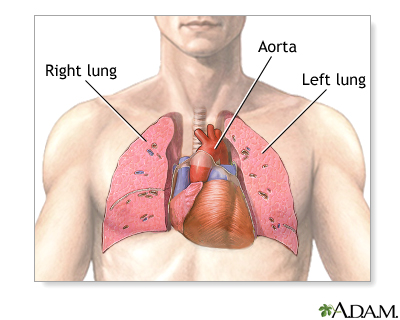
Normal anatomy
Presentation
-
Respiratory system - illustration
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Respiratory system
illustration
-
Primary pulmonary hypertension - illustration
Pulmonary hypertension is the narrowing of the pulmonary arterioles within the lung. The narrowing of the arteries creates resistance and an increased work load for the heart. The heart becomes enlarged from pumping blood against the resistance. Some symptoms include chest pain, weakness, shortness of breath, and fatigue. The goal of treatment is control of the symptoms, although the disease usually develops into congestive heart failure.
Primary pulmonary hypertension
illustration
-
Normal anatomy
Presentation
-
Pulmonary hypertension
(Alt. Medicine)
-
Scleroderma
(In-Depth)
-
Chronic obstructive pulmonary disease
(Alt. Medicine)
-
Chronic obstructive pulmonary disease
(In-Depth)
-
Sickle cell disease
(In-Depth)
-
Stroke
(In-Depth)
-
Heart failure
(In-Depth)
-
Myocardial infarction
(Alt. Medicine)
-
Alpha-linolenic acid
(Alt. Medicine)
-
Edema
(Alt. Medicine)
Review Date: 1/30/2016
Reviewed By: Denis Hadjiliadis, MD, MHS, Associate Professor of Medicine, Pulmonary, Allergy and Critical Care, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.