Sickle cell anemia
Anemia - sickle cell; Hemoglobin SS disease (Hb SS); Sickle cell disease
Sickle cell anemia is a disease passed down through families. The red blood cells that are normally shaped like a disc take on a sickle or crescent shape. Red blood cells carry oxygen throughout the body.
Causes
Sickle cell anemia is caused by an abnormal type of hemoglobin called hemoglobin S. Hemoglobin is a protein inside red blood cells that carries oxygen.
- Hemoglobin S changes the red blood cells. The red blood cells become fragile and shaped like crescents or sickles.
- The abnormal cells deliver less oxygen to the body's tissues.
- They can also easily get stuck in small blood vessels and break into pieces. This can interrupt healthy blood flow and cut down even more on the amount of oxygen flowing to body tissues.
Sickle cell anemia is inherited from both parents. If you get the sickle cell gene from only 1 parent, you will have sickle cell trait . People with sickle cell trait do not have the symptoms of sickle cell anemia.
Sickle cell trait
The sickle cell test looks for the abnormal hemoglobin in the blood that causes the disease sickle cell anemia.

Sickle cell disease is much more common in people of African and Mediterranean descent. It is also seen in people from South and Central America, the Caribbean, and the Middle East.
Symptoms
Symptoms usually do not occur until after the age of 4 months.
Almost all people with sickle cell anemia have painful episodes called crises. These can last from hours to days. Crises can cause pain in the lower back, leg, joints, and chest.
Some people have 1 episode every few years. Others have many episodes each year. The crises can be severe enough to require a hospital stay.
When the anemia becomes more severe, symptoms may include:
-
Fatigue
Fatigue
Fatigue is a feeling of weariness, tiredness, or lack of energy.
Read Article Now Book Mark Article - Paleness
- Rapid heart rate
- Shortness of breath
-
Yellowing of the eyes and skin (
jaundice
)
Jaundice
Jaundice is a yellow color of the skin, mucus membranes, or eyes. The yellow coloring comes from bilirubin, a byproduct of old red blood cells. Jau...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Younger children with sickle cell anemia have attacks of abdominal pain .
Abdominal pain
Abdominal pain is pain that you feel anywhere between your chest and groin. This is often referred to as the stomach region or belly.

The following symptoms may occur because small blood vessels become blocked by the abnormal cells:
-
Painful and prolonged erection (
priapism
)
Priapism
Penis pain is any pain or discomfort in the penis.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Poor eyesight or blindness
- Problems with thinking or confusion caused by small strokes
-
Ulcers
on the lower legs (in adolescents and adults)
Ulcers
An ulcer is a crater-like sore on the skin or mucous membrane. Ulcers form when the top layers of skin or tissue have been removed. They can occur ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Over time, the spleen stops working. As a result, people with sickle cell anemia may have symptoms of infections such as:
-
Bone infection (
osteomyelitis
)
Osteomyelitis
Osteomyelitis is a bone infection. It is mainly caused by bacteria or other germs.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Gallbladder infection (cholecystitis)
- Lung infection (pneumonia)
- Urinary tract infection
Other signs and symptoms include:
- Delayed growth and puberty
- Painful joints caused by arthritis
- Heart or liver failure due to too much iron (from blood transfusions)
Exams and Tests
Tests commonly done to diagnose and monitor people with sickle cell anemia include:
-
Bilirubin
Bilirubin
The bilirubin blood test measures the level of bilirubin in the blood. Bilirubin is a yellowish pigment found in bile, a fluid made by the liver. Bi...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Blood oxygen saturation
-
Complete blood count (
CBC
)
CBC
A complete blood count (CBC) test measures the following:The number of red blood cells (RBC count)The number of white blood cells (WBC count)The tota...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Hemoglobin electrophoresis
Hemoglobin electrophoresis
Hemoglobin is a protein that carries oxygen in the blood. Hemoglobin electrophoresis measures the levels of the different types of this protein in t...
Read Article Now Book Mark Article -
Serum creatinine
Serum creatinine
The creatinine blood test measures the level of creatinine in the blood. This test is done to see how well your kidneys are working. Creatinine can ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Serum potassium
-
Sickle cell test
Sickle cell test
The sickle cell test looks for the abnormal hemoglobin in the blood that causes the disease sickle cell anemia.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
The goal of treatment is to manage and control symptoms, and to limit the number of crises. People with sickle cell disease need ongoing treatment, even when not having a crisis.
People with this condition should take folic acid supplements. Folic acid helps make new red blood cells.
Treatment for a sickle cell crisis includes:
- Blood transfusions (may also be given regularly to prevent stroke)
- Pain medicines
- Plenty of fluids
Other treatments for sickle cell anemia may include:
- Hydroxyurea (Hydrea), which helps reduce the number of pain episodes (including chest pain and breathing problems) in some people
- Antibiotics, which help prevent bacterial infections that are common in children with sickle cell disease
- Medicines that reduce the amount of iron in the body.
Treatments that may be needed to manage complications of sickle cell anemia include:
-
Dialysis or
kidney transplant
for kidney disease
Kidney transplant
A kidney transplant is surgery to place a healthy kidney into a person with kidney failure.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Counseling for psychological complications
-
Gallbladder removal
in people with gallstone disease
Gallbladder removal
Open gallbladder removal is surgery to remove the gallbladder through a large cut in your abdomen.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Hip replacement
for
avascular necrosis
of the hip
Hip replacement
Hip joint replacement is surgery to replace all or part of the hip joint with a man-made joint. The artificial joint is called a prosthesis....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleAvascular necrosis
Osteonecrosis is bone death caused by poor blood supply. It is most common in the hip and shoulder, but can affect other large joints such as the kn...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Surgery for eye problems
- Treatment for overuse or abuse of narcotic pain medicines
- Wound care for leg ulcers
Bone marrow or stem cell transplants can cure sickle cell anemia, but this treatment is not an option for most people. Sickle cell anemia people often cannot find well-matched stem cell donors.
People with sickle cell disease should have the following vaccinations to lower the risk of infection:
- Haemophilus influenzae vaccine (Hib)
- Pneumococcal conjugate vaccine (PCV)
- Pneumococcal polysaccharide vaccine (PPV)
Support Groups
Joining a support group where members share common issues can relieve the stress of a chronic disease.
Support group
The following organizations are good resources for information on sickle cell anemia:American Sickle Cell Anemia Association -- www. ascaa. orgNation...
Outlook (Prognosis)
In the past, people with sickle cell disease often died between ages 20 and 40. Thanks to a modern care, people now can live to the age of 50 and beyond.
Causes of death include organ failure and infection.
When to Contact a Medical Professional
Call your health care provider if you have:
- Any symptoms of infection (fever, body aches, headache, fatigue)
- Pain crises
- Painful and long-term erection (in men)
References
Heeney MM, Ware RE. Sickle cell disease. In: Orkin SH, Fisher DE, Ginsburg D, Look AT, Lux SE, Nathan DG, eds. Nathan and Oski's Hematology and Oncology of Infancy and Childhood . 6th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 20.
National Heart Lung and Blood Institute. Evidence-based management of sickle cell disease: expert panel report 2014. www.nhlbi.nih.gov/sites/www.nhlbi.nih.gov/files/sickle-cell-disease-report.pdf . Accessed February 19, 2016.
Steinberg MH. Sickle cell disease and other hemoglobinopathies. In: Goldman L, Schafer AI, eds. Goldman's Cecil Medicine . 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 163.
-
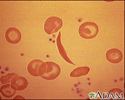
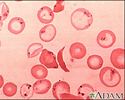
Red blood cells, sickle cell - illustration
Sickle cell anemia is an inherited blood disease in which the red blood cells produce abnormal pigment (hemoglobin). The abnormal hemoglobin causes deformity of the red blood cells into crescent or sickle-shapes, as seen in this photomicrograph.
Red blood cells, sickle cell
illustration
-
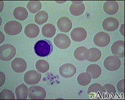
Red blood cells, normal - illustration
This photomicrograph shows normal red blood cells (RBCs) as seen in the microscope after staining.
Red blood cells, normal
illustration
-
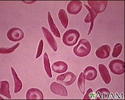
Red blood cells, multiple sickle cells - illustration
Sickle cell anemia is an inherited disorder in which abnormal hemoglobin (the red pigment inside red blood cells) is produced. The abnormal hemoglobin causes red blood cells to assume a sickle shape, like the ones seen in this photomicrograph.
Red blood cells, multiple sickle cells
illustration
-
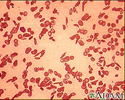
Red blood cells, sickle cells - illustration
These crescent or sickle-shaped red blood cells (RBCs) are present with Sickle cell anemia, and stand out clearly against the normal round RBCs. These abnormally shaped cells may become entangled and block blood flow in the small blood vessels (capillaries).
Red blood cells, sickle cells
illustration
-
Red blood cells, sickle and pappenheimer - illustration
This photomicrograph of red blood cells (RBCs) shows both sickle-shaped and Pappenheimer bodies.
Red blood cells, sickle and pappenheimer
illustration
-
Formed elements of blood - illustration
Blood transports oxygen and nutrients to body tissues and returns waste and carbon dioxide. Blood distributes nearly everything that is carried from one area in the body to another place within the body. For example, blood transports hormones from endocrine organs to their target organs and tissues. Blood helps maintain body temperature and normal pH levels in body tissues. The protective functions of blood include clot formation and the prevention of infection.
Formed elements of blood
illustration
-
Blood cells - illustration
Blood is comprised of red blood cells, platelets, and various white blood cells.
Blood cells
illustration
-
Red blood cells, sickle cell - illustration
Sickle cell anemia is an inherited blood disease in which the red blood cells produce abnormal pigment (hemoglobin). The abnormal hemoglobin causes deformity of the red blood cells into crescent or sickle-shapes, as seen in this photomicrograph.
Red blood cells, sickle cell
illustration
-
Red blood cells, normal - illustration
This photomicrograph shows normal red blood cells (RBCs) as seen in the microscope after staining.
Red blood cells, normal
illustration
-
Red blood cells, multiple sickle cells - illustration
Sickle cell anemia is an inherited disorder in which abnormal hemoglobin (the red pigment inside red blood cells) is produced. The abnormal hemoglobin causes red blood cells to assume a sickle shape, like the ones seen in this photomicrograph.
Red blood cells, multiple sickle cells
illustration
-
Red blood cells, sickle cells - illustration
These crescent or sickle-shaped red blood cells (RBCs) are present with Sickle cell anemia, and stand out clearly against the normal round RBCs. These abnormally shaped cells may become entangled and block blood flow in the small blood vessels (capillaries).
Red blood cells, sickle cells
illustration
-
Red blood cells, sickle and pappenheimer - illustration
This photomicrograph of red blood cells (RBCs) shows both sickle-shaped and Pappenheimer bodies.
Red blood cells, sickle and pappenheimer
illustration
-
Formed elements of blood - illustration
Blood transports oxygen and nutrients to body tissues and returns waste and carbon dioxide. Blood distributes nearly everything that is carried from one area in the body to another place within the body. For example, blood transports hormones from endocrine organs to their target organs and tissues. Blood helps maintain body temperature and normal pH levels in body tissues. The protective functions of blood include clot formation and the prevention of infection.
Formed elements of blood
illustration
-
Blood cells - illustration
Blood is comprised of red blood cells, platelets, and various white blood cells.
Blood cells
illustration
-
Sickle cell disease
(In-Depth)
-
Anemia
(Alt. Medicine)
Review Date: 2/1/2016
Reviewed By: Todd Gersten, MD, Hematology/Oncology, Florida Cancer Specialists & Research Institute, Wellington, FL. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.