Spinal stenosis
Pseudo-claudication; Central spinal stenosis; Foraminal spinal stenosis; Degenerative spine disease; Back pain - spinal stenosis; Low back pain - stenosis; LBP - stenosis
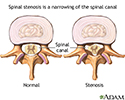
Spinal stenosis is narrowing of the spinal column that causes pressure on the spinal cord, or narrowing of the openings (called neural foramina) where spinal nerves leave the spinal column.
Causes
Spinal stenosis usually occurs as a person ages.
- The spinal disks become drier and start to bulge.
- The bones and ligaments of the spine thicken or grow larger. This is caused by arthritis or long-term swelling.
Spinal stenosis may also be caused by:
-
Arthritis
of the spine, usually in middle-aged or older people
Arthritis
Arthritis is inflammation of one or more joints. A joint is the area where 2 bones meet. There are more than 100 different types of arthritis....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Bone diseases, such as
Paget disease
Paget disease
Paget disease is a disorder that involves abnormal bone destruction and regrowth. This results in deformity of the affected bones.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Defect or growth in the spine that was present from birth
-
Herniated
or slipped disk, which often happened in the past
Herniated
A herniated (slipped) disk occurs when all or part of a disk is forced through a weakened part of the disk. This may place pressure on nearby nerves...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Injury that causes pressure on the nerve roots or the spinal cord
-
Tumors
in the spine
Tumors
A spinal tumor is a growth of cells (mass) in or surrounding the spinal cord.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Fracture or injury of a spinal bone
Symptoms
Symptoms often get worse slowly over time. Most often, symptoms will be on one side of the body, but may involve both legs.
Symptoms include:
-
Numbness
, cramping, or pain in the back, buttocks, thighs, or calves, or in the neck, shoulders, or arms
Numbness
Numbness and tingling are abnormal sensations that can occur anywhere in your body, but they are often felt in your fingers, hands, feet, arms, or le...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Weakness of part of a leg or arm
Symptoms are more likely to be present or get worse when you stand or walk. They often lessen or disappear when you sit down or lean forward. Most people with spinal stenosis cannot walk for a long period.
More serious symptoms include:
- Difficulty or poor balance when walking
- Problems controlling urine or bowel movements
Exams and Tests
During a physical exam, your doctor will try to find the location of the pain and determine how it affects your movement. You will be asked to:
- Sit, stand, and walk. While you walk, your doctor may ask you to try walking on your toes and then your heels.
- Bend forward, backward, and sideways. Your pain may worsen with these movements.
- Lift your legs straight up while lying down. If the pain is worse when you do this, you may have sciatica, especially if you also feel numbness or tingling in one of your legs.
Your doctor will also move your legs in different positions, including bending and straightening your knees. This is to check your strength and ability to move.
To test nerve function, the doctor uses a rubber hammer to check your reflexes. To test how well your nerves sense feeling, the doctor touches your legs in many places with a pin, cotton swab, or feather.
A brain and nervous system (neurologic) examination helps confirm leg weakness and decreased sensation in the legs. The following tests may be done:
Decreased sensation
Numbness and tingling are abnormal sensations that can occur anywhere in your body, but they are often felt in your fingers, hands, feet, arms, or le...

-
EMG
EMG
Electromyography (EMG) is a test that checks the health of the muscles and the nerves that control the muscles.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Spinal MRI
or
spinal CT
scan
Spinal MRI
A lumbar magnetic resonance imaging (MRI) scan uses energy from strong magnets to create pictures of the lower part of the spine (lumbar spine). An M...
Read Article Now Book Mark ArticleSpinal CT
A lumbosacral spine CT is a computed tomography scan of the lower spine and surrounding tissues.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
X-ray of the spine
X-ray of the spine
A thoracic spine x-ray is an x-ray of the twelve chest (thoracic) bones (vertebrae). The vertebrae are separated by flat pads of cartilage called di...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
Your doctor and other health professionals will help you manage your pain and keep you as active as possible.
- Your doctor may refer you for physical therapy. The physical therapist will teach you stretches and exercises that make your back muscles stronger.
- You may also see a chiropractor , a massage therapist, and someone who performs acupuncture. Sometimes, a few visits will help your back or neck pain.
- Cold packs and heat therapy may help your pain during flare-ups.
Treatments for back pain caused by spinal stenosis include:
-
Medicines that may help with your back pain
.
Medicines that may help with your back ...
Back pain often goes away on its own over several weeks. In some people, back pain persists. It may not go away completely or it may get more painf...
Read Article Now Book Mark Article -
A type of talk therapy called
cognitive behavioral therapy
to help you better understand your pain and teach you how to manage back pain.
Cognitive behavioral therapy
Nonspecific back pain - cognitive behavioral; Backache - chronic - cognitive behavioral; Lumbar pain - chronic - cognitive behavioral; Pain - back - ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - An epidural spinal injection (ESI) involves injecting medicine directly into the space around your spinal nerves or spinal cord.
Spinal stenosis symptoms often become worse over time, but this may happen slowly. If the pain does not respond to these treatments, or you lose movement or feeling, you may need surgery.
- Surgery is done to relieve pressure on the nerves or spinal cord.
- You and your doctor can decide when you need to have surgery for these symptoms.
Surgery may include removing a bulging disk , removing part of the vertebra bone , or widening the opening where your spinal nerves are located.
Removing a bulging disk
Spinal fusion is surgery to permanently join together two or more bones in the spine so there is no movement between them. These bones are called ve...

Removing part of the vertebra bone
Laminectomy is surgery to remove the lamina. This is part of the bone that makes up a vertebra in the spine. Laminectomy may also be done to remove...
Widening the opening where your spinal ...
Foraminotomy is surgery that widens the opening in your back where nerve roots leave your spinal canal. You may have a narrowing of the nerve openin...
During some spinal surgeries, the surgeon will remove some bone to create more room for your spinal nerves or spinal column. The surgeon will then fuse some of the spine bones to make your spine more stable. But this will make your back more stiff.
Outlook (Prognosis)
Many people with spinal stenosis are able to be active with the condition, although they may need to make some changes in their activities or work.
Spine surgery will often partly or fully relieve symptoms in your legs or arms. It is hard to predict if you will improve and how much relief surgery will provide.
- People who had long-term back pain before their surgery are likely to have some pain after surgery.
- If you needed more than one kind of back surgery, you may be more likely to have future problems.
- The area of the spinal column above and below a spinal fusion are more likely to be stressed and have problems and arthritis in the future. This may lead to more surgeries later.
In rare cases, injuries caused by pressure on the nerves are permanent, even if the pressure is relieved.
When to Contact a Medical Professional
Call your health care provider if you have symptoms of spinal stenosis.
More serious symptoms that need prompt attention include:
- Difficulty or poor balance when walking
- Worsening numbness and weakness of your limb
- Problems controlling urine or bowel movements
- Problems urinating or having a bowel movement
References
Chou R, Baisden J, Carragee EJ, Resnick DK, Shaffer WO, Loeser JD. Surgery for low back pain: a review of the evidence for an American Pain Society clinical practice guideline. Spine (Phila Pa 1976) . 2009;34(10):1094-1109. PMID: 19363455 www.ncbi.nlm.nih.gov/pubmed/19363455 .
Försth P, Ólafsson G, Carlsson T, et al. A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Engl J Med . 2016;374(15):1413-1423. PMID: 27074066 www.ncbi.nlm.nih.gov/pubmed/27074066 .
Ghogawala Z, Dziura J, Butler WE, et al. Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. N Engl J Med . 2016;374(15):1424-1434. PMID: 27074067 www.ncbi.nlm.nih.gov/pubmed/27074067 .
Kreiner DS, Shaffer WO, Baisden JL, et al. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update). Spine J . 2013;13(7):734-743. PMID: 23830297 www.ncbi.nlm.nih.gov/pubmed/23830297 .
Van Zundert J, Vanelderen P, Kessels AG. Re: Chou R, Atlas SJ, Stanos SP, et al. Nonsurgical interventional therapies for low back pain: a review of the evidence for an American Pain Society clinical practice guideline. Spine (Phila Pa 1976) . 2009;34:1078-1093. Spine (Phila Pa 1976) . 2010;35(7):841. PMID: 20357643 www.ncbi.nlm.nih.gov/pubmed/20357643 .
Zacharia I, Lopez E. Lumbar spinal stenosis. In: Frontera WR, Silver JK, Rizzo TD, eds. Essentials of Physical Medicine and Rehabilitation . 3rd ed. Philadelphia, PA: Elsevier Saunders; 2014:chap 50.
-
Sciatic nerve - illustration
The main nerve traveling down the leg is the sciatic nerve. Pain associated with the sciatic nerve usually originates higher along the spinal cord when nerve roots become compressed or damaged from narrowing of the vertebral column or from a slipped disk. Symptoms can include tingling, numbness, or pain, which radiates to the buttocks legs and feet.
Sciatic nerve
illustration
-
Spinal stenosis - illustration
Spinal stenosis is narrowing of the spinal canal. This can develop as you age from drying out and shrinking of the disk spaces. (The disks are 80% water.) If this happens, even a minor injury can cause inflammation of the disk and put pressure on the nerve. You can feel pain anywhere along your back or leg(s) that this nerve supplies.
Spinal stenosis
illustration
-
Spinal stenosis - illustration
Spinal stenosis is a narrowing of the lumbar or cervical spinal canal. The narrowing can cause compression on nerve roots resulting in pain or weakness of the legs. Medications or steroid injections are often administered to reduce inflammation. If the pain is persistent and does not respond to these conservative measures, surgery is considered to relieve the pressure on the nerves.
Spinal stenosis
illustration
-
Sciatic nerve - illustration
The main nerve traveling down the leg is the sciatic nerve. Pain associated with the sciatic nerve usually originates higher along the spinal cord when nerve roots become compressed or damaged from narrowing of the vertebral column or from a slipped disk. Symptoms can include tingling, numbness, or pain, which radiates to the buttocks legs and feet.
Sciatic nerve
illustration
-
Spinal stenosis - illustration
Spinal stenosis is narrowing of the spinal canal. This can develop as you age from drying out and shrinking of the disk spaces. (The disks are 80% water.) If this happens, even a minor injury can cause inflammation of the disk and put pressure on the nerve. You can feel pain anywhere along your back or leg(s) that this nerve supplies.
Spinal stenosis
illustration
-
Spinal stenosis - illustration
Spinal stenosis is a narrowing of the lumbar or cervical spinal canal. The narrowing can cause compression on nerve roots resulting in pain or weakness of the legs. Medications or steroid injections are often administered to reduce inflammation. If the pain is persistent and does not respond to these conservative measures, surgery is considered to relieve the pressure on the nerves.
Spinal stenosis
illustration
Review Date: 7/13/2015
Reviewed By: C. Benjamin Ma, MD, Professor, Chief, Sports Medicine and Shoulder Service, UCSF Department of Orthopaedic Surgery, San Francisco, CA. Internal review and update on 09/01/2016 by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.