Hip joint replacement
Hip arthroplasty; Total hip replacement; Hip hemiarthroplasty; Arthritis - hip replacement; Osteoarthritis - hip replacement
Hip joint replacement is surgery to replace all or part of the hip joint with a man-made joint. The artificial joint is called a prosthesis .
Prosthesis
A prosthesis is a device designed to replace a missing part of the body or to make a part of the body work better. Diseased or missing eyes, arms, h...

Description
Your hip joint is made up of 2 major parts. One or both parts may be replaced during surgery:
- The hip socket (a part of the pelvic bone called the acetabulum)
- The upper end of the thighbone (called the femoral head)
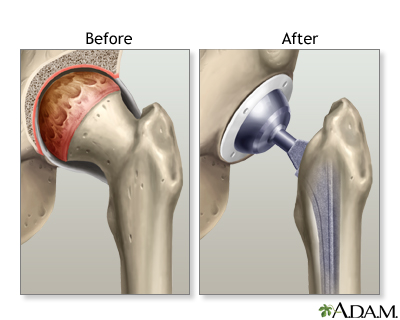
The new hip that replaces the old one is made up of these parts:
- A socket, which is usually made of strong metal.
- A liner, which fits inside the socket. It is usually plastic. Some surgeons are now trying other materials, like ceramic or metal. The liner allows the hip to move smoothly.
- A metal or ceramic ball that will replace the round head (top) of your thigh bone.
- A metal stem that is attached to the thigh bone to anchor the joint.
You will not feel any pain during surgery. You will have 1 of 2 types of anesthesia:
-
General anesthesia
. This means you will be asleep and unable to feel pain.
General anesthesia
General anesthesia is treatment with certain medicines that puts you into a deep sleep so you do not feel pain during surgery. After you receive the...
Read Article Now Book Mark Article -
Regional (
spinal or epidural
) anesthesia. Medicine is put into your back to make you numb below your waist. You will also get medicine to make you sleepy. And you may get medicine that will make you forget about the procedure, even though you will not be fully asleep.
Spinal or epidural
Spinal and epidural anesthesia are medicines that numb parts of your body to block pain. They are given through shots in or around the spine....
Read Article Now Book Mark Article
After you receive anesthesia, your surgeon will make a surgical cut to open up your hip joint. This cut is often over the buttocks. Then your surgeon will:
- Cut and remove the head of your thigh bone.
- Clean out your hip socket and remove the rest of the cartilage and damaged or arthritic bone.
- Put the new hip socket in place, a liner is then placed in the new socket.
- The metal stem is then inserted into your thigh bone.
- Place the correct-sized ball for the new joint.
- Secure all of the new parts in place, sometimes with a special cement.
- Repair the muscles and tendons around the new joint.
- Close the surgical wound.
This surgery takes about 1 to 3 hours.
Why the Procedure Is Performed
The most common reason to have this surgery is to relieve arthritis . Severe arthritis pain can limit your activities.
Arthritis
Arthritis is inflammation of one or more joints. A joint is the area where 2 bones meet. There are more than 100 different types of arthritis....

Most of the time, hip joint replacement is done in people age 60 and older. Many people who have this surgery are younger. Younger people who have a hip replaced may put extra stress on the artificial hip. That extra stress can cause it to wear out earlier than in older people. Part or all of the joint may need to be replaced again if that happens.
Your doctor may recommend a hip replacement for these problems:
- You can't sleep through the night because of hip pain.
- Your hip pain has not gotten better with other treatments.
- Hip pain limits or prevents you from doing your normal activities, such as bathing, preparing meals, doing household chores, and walking.
- You have problems walking that require you to use a cane or walker.
Other reasons for replacing the hip joint are:
-
Fractures
in the thigh bone. Older adults often have a hip replacement for this reason.
Fractures
If more pressure is put on a bone than it can stand, it will split or break. A break of any size is called a fracture. If the broken bone punctures...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Hip joint tumors.
Before the Procedure
Always tell your provider what drugs you are taking, even drugs, supplements, or herbs you bought without a prescription.
During the 2 weeks before your surgery:
-
Prepare your home
.
Prepare your home
Hip or knee surgery - getting your home ready; Osteoarthritis - knee
Read Article Now Book Mark Article - You may be asked to stop taking drugs that make it harder for your blood to clot. These include aspirin, ibuprofen (Advil, Motrin), naproxen (Naprosyn, Aleve), blood thinners such as warfarin (Coumadin), and other drugs.
- You may also need to stop taking medicine that can make you more likely to get an infection. This includes methotrexate, Enbrel, and other medicines that suppress your immune system.
- Ask your provider which drugs you should still take on the day of your surgery.
- If you have diabetes, heart disease, or other medical conditions, your surgeon will ask you to see the provider who treats you for these conditions.
- Tell your provider if you have been drinking a lot of alcohol, more than 1 or 2 drinks a day.
- If you smoke, you need to stop. Ask your provider or nurse for help. Smoking will slow down wound and bone healing.
- Always let your provider know about any cold, flu, fever, herpes breakout, or other illness you have before your surgery.
- You may want to visit a physical therapist to learn some exercises to do before surgery and to practice using crutches or a walker.
- Set up your home to make everyday tasks easier.
Practice using a cane, walker , crutches , or wheelchair correctly to:
- Get in and out of the shower
- Go up and down stairs
- Sit down to use the toilet and stand up after using the toilet
- Use the shower chair
On the day of your surgery:
- You will usually be asked not to drink or eat anything for 6 to 12 hours before the procedure.
- Take the drugs your provider told you to take with a small sip of water.
Your provider will tell you when to arrive at the hospital.
After the Procedure
You will stay in the hospital for 1 to 3 days. During that time you will recover from your anesthesia, and from the surgery itself. You will be asked to start moving and walking as soon as the first day after surgery.
Stay in the hospital
You will stay in the hospital for 2 to 3 days after having hip or knee joint replacement surgery. During that time you will recover from your anesth...
Some people need a short stay in a rehabilitation center after they leave the hospital and before they go home . At a rehab center, you will learn how to safely do your daily activities on your own . Home health services are also available.
Before they go home
Hip arthroplasty - discharge; Total hip replacement - discharge; Hip hemiarthroplasty - discharge; Osteoarthritis - hip replacement discharge...
Daily activities on your own
Hip arthroplasty - precautions; Hip replacement - precautions; Osteoarthritis - hip; Osteoarthritis - knee
Outlook (Prognosis)
Hip replacement surgery results are often excellent. Most or all of your pain and stiffness should go away.
Some people may have problems with infection, loosening, or even dislocation of the new hip joint.
Over time, the artificial hip joint can loosen. This can happen after as long as 15 to 20 years. You may need a second replacement.
Younger, more active people may wear out parts of their new hip. It may need to be replaced before the artificial hip loosens.
References
Cabrera JA, Cabrera AL. Total hip replacement. In: Frontera WR, Silver JK, Rizzo TD, eds. Essentials of Physical Medicine and Rehabilitation . 3rd ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 61.
Foran JRH. OrthoInfo: total hip replacement. American Academy of Orthopaedic Surgeons . Updated August 2015. orthoinfo.aaos.org/topic.cfm?topic=a00377 . Accessed May 9, 2016.
Harkess JW, Crockarell JR. Arthroplasty of the hip. In: Canale ST, Beaty JH, eds. Campbell's Operative Orthopaedics . 12th ed. Philadelphia, PA: Elsevier Mosby; 2013:chap 3.
Preventing venous thromboembolic disease in patients undergoing elective hip and knee arthopolasty: Evidence-based guideline and evidence report. American Association of Orthopaedic Surgeons . 2011. www.aaos.org/research/guidelines/VTE/VTE_full_guideline.pdf .
Svege I, Nordsletten L, Fernandes L, Risberg MA. Exercise therapy may postpone total hip replacement surgery in patients with hip osteoarthritis: a long-term follow-up of a randomised trial. Ann Rheum Dis . 2015;74(1):164-9. PMID: 24255546 www.ncbi.nlm.nih.gov/pubmed/24255546 .
-
Hip joint replacement
Animation
-
Hip fracture - illustration
Hip fractures occur as a result of major or minor trauma. In elderly patients with bones weakened by osteoporosis, relatively little trauma, even walking, may result in a hip fracture.
Hip fracture
illustration
-
Osteoarthritis vs. rheumatoid arthritis - illustration
Osteoarthritis is a deterioration of cartilage and overgrowth of bone often due to "wear and tear". Rheumatoid arthritis is the inflammation of a joint's connective tissues, such as the synovial membranes, which leads to the destruction of the articular cartilage.
Osteoarthritis vs. rheumatoid arthritis
illustration
-
Hip joint replacement - Series
Presentation
-
Hip fracture - illustration
Hip fractures occur as a result of major or minor trauma. In elderly patients with bones weakened by osteoporosis, relatively little trauma, even walking, may result in a hip fracture.
Hip fracture
illustration
-
Osteoarthritis vs. rheumatoid arthritis - illustration
Osteoarthritis is a deterioration of cartilage and overgrowth of bone often due to "wear and tear". Rheumatoid arthritis is the inflammation of a joint's connective tissues, such as the synovial membranes, which leads to the destruction of the articular cartilage.
Osteoarthritis vs. rheumatoid arthritis
illustration
-
Hip joint replacement - Series
Presentation
Review Date: 4/17/2016
Reviewed By: C. Benjamin Ma, MD, Professor, Chief, Sports Medicine and Shoulder Service, UCSF Department of Orthopaedic Surgery, San Francisco, CA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.