Lung transplant
Solid organ transplant - lung
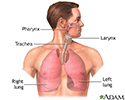
Lung transplant is surgery to replace one or both diseased lungs with healthy lungs from a human donor.
Description
In most cases, the new lung or lungs are usually donated by a person who is under age 65 and brain-dead, but is still on life-support. The donor tissue must be matched as closely as possible to your tissue type. This reduces the chance that the body will reject the transplant .
Transplant
Transplantation is a procedure that is done to replace one of your organs with a healthy one from someone else. The surgery is only one part of a co...
Lungs can also be given by living donors. Two or more people are needed. Each person donates a segment (lobe) of their lung. This forms an entire lung for the person who is receiving it.
During lung transplant surgery, you are asleep and pain-free (under general anesthesia ). A surgical cut is made in the chest. Lung transplant surgery is often done with the use of a heart-lung machine. This device does the work of your heart and lungs while your heart and lungs are stopped for the surgery.
General anesthesia
General anesthesia is treatment with certain medicines that puts you into a deep sleep so you do not feel pain during surgery. After you receive the...
- For single lung transplants, the cut is made on the side of your chest where the lung will be transplanted. The operation takes 4 to 8 hours. In most cases, the lung with the worst function is removed.
- For double lung transplants, the cut is made below the breast and reaches to both sides of the chest. Surgery takes 6 to 12 hours.
After the cut is made, the major steps during lung transplant surgery include:
- One or both of your lungs are removed. For people who are having a double lung transplant, most or all of the steps from the first side are completed before the second side is done.
- The main blood vessels and airway of the new lung are sewn to your blood vessels and airway. The donor lobe or lung is stitched (sutured) into place. Chest tubes are inserted to drain air, fluid, and blood out of the chest for several days to allow the lungs to fully re-expand.
Sometimes, heart and lung transplants are done at the same time (heart-lung transplant) if the heart is also diseased.
Why the Procedure Is Performed
In most cases, a lung transplant is done only after all other treatments for lung failure are unsuccessful. Lung transplants may be recommended for people under age 65 who have severe lung disease. Some examples of diseases that may require a lung transplant are:
-
Cystic fibrosis
Cystic fibrosis
Cystic fibrosis is a disease that causes thick, sticky mucus to build up in the lungs, digestive tract, and other areas of the body. It is one of th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Damage to the arteries of the lung because of a
defect in the heart at birth (congenital defect
)
Defect in the heart at birth (congenita...
Congenital heart disease (CHD) is a problem with the heart's structure and function that is present at birth.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Destruction of the large airways and lung (
bronchiectasis
)
Bronchiectasis
Bronchiectasis is a disease in which the large airways in the lungs are damaged. This causes the airways to become wider. Bronchiectasis can be pres...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Emphysema or
chronic obstructive pulmonary disease (COPD)
Chronic obstructive pulmonary disease (...
Chronic obstructive pulmonary disease (COPD) is a common lung disease. Having COPD makes it hard to breathe. There are two main forms of COPD:Chroni...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Lung conditions in which the lung tissues become swollen and scarred (
interstitial lung disease
)
Interstitial lung disease
Interstitial lung disease is a group of lung disorders in which the lung tissues become inflamed and then damaged.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
High blood pressure in the arteries of the lungs (
pulmonary hypertension
)
Pulmonary hypertension
Pulmonary hypertension is high blood pressure in the arteries of the lungs. It makes the right side of the heart work harder than normal.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Sarcoidosis
Sarcoidosis
Sarcoidosis is a disease in which inflammation occurs in the lymph nodes, lungs, liver, eyes, skin, or other tissues.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Lung transplant may not be done for people who:
-
Are too sick or
badly nourished
to go through the procedure
Badly nourished
Malnutrition is the condition that occurs when your body does not get enough nutrients.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Continue to smoke or abuse alcohol or other drugs
-
Have active hepatitis B,
hepatitis
C, or
HIV
Hepatitis
Hepatitis is swelling and inflammation of the liver.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleHIV
Human immunodeficiency virus (HIV) is the virus that causes AIDS. When a person becomes infected with HIV, the virus attacks and weakens the immune ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Have had cancer within the past 2 years
-
Have
lung disease
that will likely affect the new lung
Lung disease
Lung disease is any problem in the lungs that prevents the lungs from working properly. There are three main types of lung disease:Airway diseases -...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Have severe disease of other organs
- Cannot reliably take their medicines
- Are unable to keep up with the hospital and health care visits and tests that are needed
Risks
Risks of lung transplant include:
-
Blood clots (
deep venous thrombosis
)
Deep venous thrombosis
Deep vein thrombosis (DVT) is a condition that occurs when a blood clot forms in a vein deep inside a part of the body. It mainly affects the large ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Diabetes
, bone thinning, or high cholesterol levels from the medicines given after a transplant
Diabetes
Diabetes is a chronic disease in which the body cannot regulate the amount of sugar in the blood.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Increased risk for infections due to anti-rejection (immunosuppression) medicines
- Damage to your kidneys, liver, or other organs from anti-rejection medicines
- Future risk of certain cancers
- Problems at the place where the new blood vessels and airways were attached
-
Rejection
of the new lung, which may happen right away, within the first 4 to 6 weeks, or over time
Rejection
Transplant rejection is a process in which a transplant recipient's immune system attacks the transplanted organ or tissue.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Before the Procedure
You will have the following tests to determine if you are a good candidate for the operation:
- Blood tests or skin tests to check for infections
-
Blood typing
Blood typing
Blood typing is a method to tell what type of blood you have. Blood typing is done so you can safely donate your blood or receive a blood transfusio...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Tests to evaluate your heart, such as
electrocardiogram
(EKG),
echocardiogram
, or
cardiac catheterization
Electrocardiogram
An electrocardiogram (ECG) is a test that records the electrical activity of the heart.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleEchocardiogram
An echocardiogram is a test that uses sound waves to create pictures of the heart. The picture and information it produces is more detailed than a s...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleCardiac catheterization
Cardiac catheterization involves passing a thin flexible tube (catheter) into the right or left side of the heart. The catheter is most often insert...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Tests to evaluate your lungs
-
Tests to look for early cancer (
Pap smear
,
mammogram
,
colonoscopy
)
Pap smear
The Pap test checks for cervical cancer. Cells scraped from the opening of the cervix are examined under a microscope. The cervix is the lower part...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleMammogram
A mammogram is an x-ray picture of the breasts. It is used to find breast tumors and cancer.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleColonoscopy
A colonoscopy is an exam that views the inside of the colon (large intestine) and rectum, using a tool called a colonoscope. The colonoscope has a sm...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Tissue typing, to help make sure your body will not reject the donated lung
Good candidates for transplant are put on a regional waiting list. Your place on the waiting list is based on a number of factors, including:
- What type of lung problems you have
- The severity of your lung disease
- The likelihood that a transplant will be successful
For most adults, the amount of time you spend on a waiting list most often does not determine how soon you get a lung. Waiting time is often at least 2 to 3 years.
While you are waiting for a new lung:
- Follow any diet your lung transplant team recommends. Stop drinking alcohol, do not smoke, and keep your weight in the recommended range.
- Take all medicines as they were prescribed. Report changes in your medicines and medical problems that are new or get worse to the transplant team.
- Follow any exercise program that you were taught during pulmonary rehabilitation.
- Keep any appointments that you have made with your regular health care provider and transplant team.
- Let the transplant team know how to contact you right away if a lung becomes available. Make sure that you can be contacted quickly and easily.
- Be prepared in advance to go to the hospital.
Before the procedure, always tell your provider:
- What drugs, vitamins, herbs, and other supplements you are taking, even ones you bought without a prescription
- If you have been drinking a lot of alcohol (more than one or two drinks a day)
Do not eat or drink anything when you are told to come to the hospital for your lung transplant. Take only the drugs that you have been told to take with a small sip of water.
After the Procedure
You should expect to stay in the hospital for 7 to 21 days after a lung transplant. You will likely spend time in the intensive care unit (ICU) right after surgery. Most centers that perform lung transplants have standard ways of treating and managing lung transplant patients.
The recovery period is about 6 months. Often, your transplant team will ask you to stay close to the hospital for the first 3 months. You will need to have regular check-ups with blood tests and x-rays for many years.
Outlook (Prognosis)
A lung transplant is a major procedure that is performed for people with life-threatening lung disease or damage.
About four out of five patients are still alive 1 year after the transplant. About two out of five transplant recipients are alive at 5 years. The highest risk of death is during the first year, mainly from problems such as rejection.
Fighting rejection is an ongoing process. The body's immune system considers the transplanted organ as an invader and may attack it.
To prevent rejection, organ transplant patients must take anti-rejection (immunosuppression) drugs. These drugs suppress the body's immune response and reduce the chance of rejection. As a result, however, these drugs also reduce the body's natural ability to fight off infections.
Immune response
The immune response is how your body recognizes and defends itself against bacteria, viruses, and substances that appear foreign and harmful....

By 5 years after a lung transplant, at least one in five people develop cancers or have problems with the heart. For most people, the quality of life is improved after a lung transplant. They have better exercise endurance and are able to do more on a daily basis.
References
Flume PA, Mogayzel PJ Jr, Robinson KA, Rosenblatt RL, Quittell L, Marshall BC; Clinical Practice Guidelines for Pulmonary Therapies Committee; Cystic Fibrosis Foundation Pulmonary Therapies Committee. Cystic fibrosis pulmonary guidelines: pulmonary complications: hemoptysis and pneumothorax. Am J Respir Crit Care Med . 2010;182(3):298-306. PMID: 20675678 www.ncbi.nlm.nih.gov/pubmed/20675678 .
Kotloff RM, Keshavjee S. Lung transplantation. In: Broaddus VC, Mason RJ, Ernst MD, et al. Murray & Nadel's Textbook of Respiratory Medicine . 6th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 106.
Putnam JB. Lung, chest wall, pleura, and mediastinum. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery . 19th ed. Philadelphia, PA: Elsevier Saunders; 2012:chap 58.
Solomon M, Grasemann H, Keshavjee S. Pediatric lung transplantation. Pediatr Clin North Am . 2010; 57(2):375-91. PMID: 20371042 www.ncbi.nlm.nih.gov/pubmed/20371042 .
Review Date: 4/13/2015
Reviewed By: Dale Mueller, MD, cardiovascular and thoracic surgeon, HeartCare Midwest; Chairman Department of Cardiovascular Medicine and Surgery, OSF St. Francis Medical Center; and Clinical Associate Professor of Surgery, University of Illinois, Peoria, IL. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.