Thrombolytic therapy
Tissue plasminogen activator; TPA; Alteplase; Reteplase; Tenecteplase; Activase thrombolytic agent; Clot-dissolving agents; Reperfusion therapy; Stroke - thrombolytic; Heart attack - thrombolytic; Acute embolism - thrombolytic; Thrombosis - thrombolytic; Lanoteplase; Staphylokinase; Streptokinase (SK); Urokinase
Thrombolytic therapy is the use of drugs to break up or dissolve blood clots, which are the main cause of both heart attacks and stroke.
Information
Thrombolytic medicines are approved for the emergency treatment of stroke and heart attack . The most commonly used drug for thrombolytic therapy is tissue plasminogen activator (tPA), but other drugs can do the same thing.
Stroke
A stroke occurs when blood flow to a part of the brain stops. A stroke is sometimes called a "brain attack. " If blood flow is cut off for longer th...

Heart attack
Most heart attacks are caused by a blood clot that blocks one of the coronary arteries. The coronary arteries bring blood and oxygen to the heart. ...

Ideally, you should receive thrombolytic medicines within the first 30 minutes after arriving at the hospital for treatment.
HEART ATTACKS
A blood clot can block the arteries to the heart. This can cause a heart attack, when part of the heart muscle dies due to a lack of oxygen being delivered by the blood.
Thrombolytics work by dissolving a major clot quickly. This helps restart blood flow to the heart and helps prevent damage to the heart muscle. Thrombolytics can stop a heart attack that would otherwise be larger or potentially deadly. Outcomes are better if you receive a thrombolytic drug within 12 hours after the heart attack starts.
The drug restores some blood flow to the heart in most people. However, the blood flow may not be completely normal and there may still be a small amount of muscle damaged. Further therapy, such as cardiac catheterization with angioplasty and stenting, may be needed.
Your health care provider will base the decisions about whether to give you a thrombolytic medicine for a heart attack on many factors. These factors include your history of chest pain and the results of an ECG test .
ECG test
An electrocardiogram (ECG) is a test that records the electrical activity of the heart.

Other factors used to determine if you are a good candidate for thrombolytics include:
- Age (older people are at increased risk of complications)
- Gender
- Medical history (including your history of a previous heart attack, diabetes, low blood pressure, or increased heart rate)
Generally, thrombolytics may not be given if you have:
- A recent head injury
- Bleeding problems
- Bleeding ulcers
- Pregnancy
- Recent surgery
- Taken blood thinning medicines such as Coumadin
- Trauma
- Uncontrolled (severe) high blood pressure
STROKES
Most strokes are caused when blood clots move to a blood vessel in the brain and block blood flow to that area. For such strokes (ischemic strokes), thrombolytics can be used to help dissolve the clot quickly. Giving thrombolytics within 3 hours of the first stroke symptoms can help limit stroke damage and disability.
The decision to give the drug is based upon:
- A brain CT scan to make sure there has not been any bleeding
- A physical exam that shows a significant stroke
- Your medical history
As in heart attacks, a clot-dissolving drug isn't usually given if you have one of the other medical problems listed above.
Thrombolytics are not given to someone who is having a stroke that involves bleeding in the brain. They could worsen the stroke by causing increased bleeding.
RISKS
Bleeding is the most common risk. It can be life threatening.
Minor bleeding from the gums or nose can occur in approximately 25% of people who receive the drug. Bleeding into the brain occurs approximately 1% of the time. This risk is the same for both stroke and heart attack patients.
If thrombolytics are felt to be too dangerous, other possible treatments for clots causing a stroke or heart attack include:
- Removal of the clot (thrombectomy)
- A procedure to open narrowed or blocked blood vessels that supply blood to the heart or the brain
CONTACT A HEALTH CARE PROVIDER OR CALL 911
Heart attacks and strokes are medical emergencies. The sooner treatment with thrombolytics begins, the better the chance for a good outcome.
References
Anderson JL. ST segment elevation acute myocardial infarction and complications of myocardial infarction. In: Goldman L, Schafer AI, eds. Goldman's Cecil Medicine . 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 73.
Goldstein LB. Ischemic cerebrovascular disease. In: Goldman L, Schafer AI, eds. Goldman's Cecil Medicine . 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 407.
Mega JL, Morrow DA. ST-segment elevation myocardial infarction: management. In: Bonow RO, Mann DL, Zipes DP, Libby P, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine . 10th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 52.
O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation . 2013;127(4):529-555. PMID: 23247303 www.ncbi.nlm.nih.gov/pubmed/23247303 .
-
Cardiac and vascular disorders: Blood clots
Animation
-
Stroke - illustration
A stroke involves loss of brain functions caused by a loss of blood circulation to areas of the brain. The blockage usually occurs when a clot or piece of atherosclerotic plaque breaks away from another area of the body and lodges within the vasculature of the brain.
Stroke
illustration
-
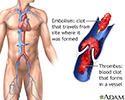
Thrombus - illustration
A thrombus is a blood clot that forms in a vessel and remains there. An embolism is a clot that travels from the site where it formed to another location in the body. Thrombi or emboli can lodge in a blood vessel and block the flow of blood in that location depriving tissues of normal blood flow and oxygen. This can result in damage, destruction (infarction), or even death of the tissues (necrosis) in that area.
Thrombus
illustration
-
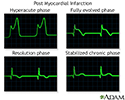
Post myocardial infarction ECG wave tracings - illustration
Various phases can be seen through ECG wave tracings following a heart attack: Hyperacute phase begins immediately after a heart attackFully evolved phase starts a few hours to days after a heart attackResolution phase appears a few weeks after a heart attackStabilized chronic phase is the last phase and typically has permanent pathological changes compared to a normal ECG tracing Hyperacute phase begins immediately after a heart attack Fully evolved phase starts a few hours to days after a heart attack Resolution phase appears a few weeks after a heart attack Stabilized chronic phase is the last phase and typically has permanent pathological changes compared to a normal ECG tracing
Post myocardial infarction ECG wave tracings
illustration
-
Stroke - illustration
A stroke involves loss of brain functions caused by a loss of blood circulation to areas of the brain. The blockage usually occurs when a clot or piece of atherosclerotic plaque breaks away from another area of the body and lodges within the vasculature of the brain.
Stroke
illustration
-
Thrombus - illustration
A thrombus is a blood clot that forms in a vessel and remains there. An embolism is a clot that travels from the site where it formed to another location in the body. Thrombi or emboli can lodge in a blood vessel and block the flow of blood in that location depriving tissues of normal blood flow and oxygen. This can result in damage, destruction (infarction), or even death of the tissues (necrosis) in that area.
Thrombus
illustration
-
Post myocardial infarction ECG wave tracings - illustration
Various phases can be seen through ECG wave tracings following a heart attack: Hyperacute phase begins immediately after a heart attackFully evolved phase starts a few hours to days after a heart attackResolution phase appears a few weeks after a heart attackStabilized chronic phase is the last phase and typically has permanent pathological changes compared to a normal ECG tracing Hyperacute phase begins immediately after a heart attack Fully evolved phase starts a few hours to days after a heart attack Resolution phase appears a few weeks after a heart attack Stabilized chronic phase is the last phase and typically has permanent pathological changes compared to a normal ECG tracing
Post myocardial infarction ECG wave tracings
illustration
Review Date: 5/5/2016
Reviewed By: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.