Hepatitis C
Sustained virologic response - hepatitis C; SVR - hepatitis C
Hepatitis C is a viral disease that leads to swelling (inflammation) of the liver.
Other types of viral hepatitis include:
-
Hepatitis A
Hepatitis A
Hepatitis A is inflammation (irritation and swelling) of the liver from the hepatitis A virus.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Hepatitis B
Hepatitis B
Hepatitis B is irritation and swelling (inflammation) of the liver due to infection with the hepatitis B virus (HBV). Other types of viral hepatitis ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Hepatitis D
Hepatitis D
Hepatitis D is a viral infection caused by the hepatitis D virus (previously called the Delta agent). It causes symptoms only in people who also hav...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Causes
Hepatitis C infection is caused by the hepatitis C virus (HCV).
You can catch hepatitis C if the blood of someone who has hepatitis C enters your body. Exposure may occur:
-
After a needle stick or sharps injury
After a needle stick or sharps injury
No definition available for this article.
Read Article Now Book Mark Article - If blood from someone who has hepatitis C contacts a cut on your skin or contacts your eyes or mouth
People at risk of hepatitis C are those who:
- Inject street drugs or share a needle with someone who has hepatitis C
- Have been on long-term kidney dialysis
- Have regular contact with blood at work (such as a health care worker)
- Have unprotected sexual contact with a person who has hepatitis C
- Were born to a mother who had hepatitis C
- Received a tattoo or acupuncture with needles that were not disinfected properly after being used on another person (risk is very low with practitioners who have a tattoo license or permit or an acupuncture license)
- Received an organ transplant from a donor who has hepatitis C
- Share personal items, such as toothbrushes and razors, with someone who has hepatitis C (less common)
-
Received a
blood transfusion
(rare in the United States since blood screening became available in 1992)
Blood transfusion
There are many reasons you may need a blood transfusion:After knee or hip replacement surgery, or other major surgery that results in blood lossAfter...
Read Article Now Book Mark Article
Symptoms
Most people who are recently infected with hepatitis C do not have symptoms in most cases. Some people have yellowing of the skin (jaundice) that goes away. Chronic infection often causes no symptoms. But tiredness, skin disorders and other problems can occur.
Persons who have long-term (chronic) infection often have no symptoms until their liver becomes scarred ( cirrhosis ). Most people with this condition are ill and have many health problems.
Cirrhosis
Cirrhosis is scarring of the liver and poor liver function. It is the last stage of chronic liver disease.

The following symptoms may occur with hepatitis C infection:
- Pain in the right upper abdomen
-
Abdominal swelling due to fluid (
ascites
)
Ascites
Ascites is the build-up of fluid in the space between the lining of the abdomen and abdominal organs.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Clay-colored or pale stools
-
Dark urine
Dark urine
Blood in your urine is called hematuria. The amount may be very small and only detected with urine tests or under a microscope. In other cases, the...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Fatigue
Fatigue
Fatigue is a feeling of weariness, tiredness, or lack of energy.
Read Article Now Book Mark Article -
Fever
Fever
Fever is the temporary increase in the body's temperature in response to a disease or illness. A child has a fever when the temperature is at or abov...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Itching
Itching
Itching is a tingling or irritation of the skin that makes you want to scratch the area. Itching may occur all over the body or only in one location...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Jaundice
- Loss of appetite
- Nausea and vomiting
Exams and Tests
Blood tests are done to check for hepatitis C:
- Enzyme immunoassay (EIA) to detect hepatitis C antibody
- Hepatitis C RNA assays to measure virus levels (viral load)
Everyone born from 1945 to 1965 (the baby boomer generation) should get a one-time test for hepatitis C.
Genetic testing is done to check for the type of hepatitis C (genotype). There are six types of the virus (genotypes 1 through 6). Test results can help your health care provider choose treatment that is best for you.
The following tests are done to identify and monitor liver damage from hepatitis C:
- Albumin level
- Liver function tests
- Prothrombin time
- Liver biopsy
Treatment
You should talk to your provider about your treatment options and when treatment should begin.
-
The goal of treatment is to rid the body of the virus. This can prevent liver damage that may lead to liver failure or
liver cancer
.
Liver cancer
Hepatocellular carcinoma is cancer that starts in the liver.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Your provider will monitor you by checking liver blood tests, viral load (the amount of HCV in your blood), imaging tests, and biopsy results.
- Treatment is especially important for people who are showing signs liver fibrosis or scarring.
Medicines used to treat hepatitis C are called antiviral drugs because they fight the HCV. Newer antiviral drugs:
- Provide a much improved cure rate
- Have fewer side effects and are easier to take
- Are taken by mouth for 8 to 24 weeks
The choice of which drug depends on the genotype of the virus you have.
A liver transplant may be recommended for people who develop cirrhosis and liver cancer. Your provider can tell you more about liver transplant.
Liver transplant
Liver transplant is surgery to replace a diseased liver with a healthy liver.

If you have hepatitis C:
- Do not take over-the-counter medicines that you have not taken before without asking your provider. Also ask about vitamins and other supplements.
- Do not use alcohol or street drugs. Alcohol can speed up the damage to your liver. It can also reduce how well medicines work.
- Ask your provider whether you need the hepatitis A and hepatitis B vaccines.
Support Groups
Joining a support group can help ease the stress of having hepatitis C. Ask your provider about liver disease resources and support groups in your area.
Liver disease resources
The following organizations are good resources for information on liver disease:American Liver Foundation -- www. liverfoundation. orgChildren's Live...

Outlook (Prognosis)
Most people (75% to 85%) who are infected with the virus develop chronic hepatitis C. This condition poses a risk for cirrhosis, liver cancer, or both. The outlook for hepatitis C depends in part on the genotype.
A good response to treatment occurs when the virus can no longer be detected in the blood 12 weeks or more after treatment. This is called "sustained virologic response" (SVR). Up to 90% of those treated for some genotypes have this type of response.
Some people do not respond to initial treatment. They may need to be re-treated with a different drug regimen.
Also, some people can become re-infected or infected with a different genotype strain.
When to Contact a Medical Professional
Call your provider if:
- You develop symptoms of hepatitis
- You believe you have been exposed to the HCV
Prevention
Steps that can be taken to help prevent the spread of hepatitis C from one person to another include:
Prevent the spread of hepatitis C
Hepatitis B and hepatitis C infections cause irritation and swelling of the liver. You should take steps to prevent catching or spreading these viru...
- Health care workers should follow precautions when handling blood.
- Do not share needles with anyone.
- Do not get tattoos or body piercings or receive acupuncture from someone who does not have a permit or license.
- Do not share personal items, such as razors and toothbrushes.
- Practice safer sex.
If you or your partner is infected with hepatitis C and you have been in a stable and monogamous (no other partners) relationship, the risk of giving the virus to, or getting the virus from, the other person is low.
HCV cannot be spread by casual contact, such as holding hands, kissing, coughing or sneezing, breastfeeding, sharing eating utensils or drinking glasses.
Currently there is no vaccine for hepatitis C.
References
Afdhal N, Zeuzem S, Kwo P, et al. Ledipasvir and sofosbuvir for untreated HCV genotype 1 infection. N Engl J Med . 2014;370(20):1889-1898. PMID: 24725239 www.ncbi.nlm.nih.gov/pubmed/24725239 .
Ghany MG, Strader DB, Thomas DL, Seeff LB; American Association for the Study of Liver Diseases. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology . 2009;49(4):1335-1374. PMID: 19330875 www.ncbi.nlm.nih.gov/pubmed/19330875 .
Kohli A, Shaffer A, Sherman A, Kottilil S. Treatment of hepatitis C: a systematic review. JAMA . 2014;312(6):631-640. PMID: 25117132 www.ncbi.nlm.nih.gov/pubmed/25117132 .
Lawitz E, Sulkowski MS, Ghalib R, et al. Simeprevir plus sofosbuvir, with or without ribavirin, to treat chronic infection with hepatitis C virus genotype 1 in non-responders to pegylated interferon and ribavirin and treatment-naive patients: the COSMOS randomised study. Lancet . 2014;384(9956):1756-1765. PMID: 25078309 www.ncbi.nlm.nih.gov/pubmed/25078309 .
Moyer VA; U.S. Preventive Services Task Force. Screening for hepatitis C virus infection in adults. U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med . 2013;159(5):349-357. PMID: 23798026 www.ncbi.nlm.nih.gov/pubmed/23798026 .
Ray SC, Thomas DL. Hepatitis C. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases . 8th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 156.
Rosen HR. Clinical practice. Chronic hepatitis C infection. N Engl J Med . 2011;364(25):2429-38. PMID: 21696309 www.ncbi.nlm.nih.gov/pubmed/21696309 .
Wedemeyer H. Hepatitis C. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 10th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 80.
-
Hepatitis C
Animation
-
Digestive system - illustration
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
Digestive system
illustration
-
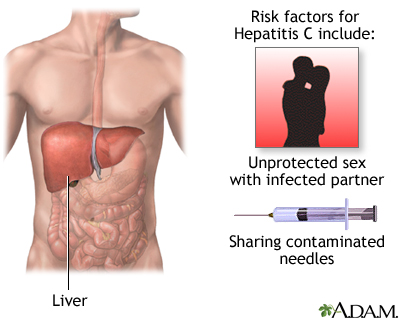
Hepatitis C - illustration
Hepatitis C is a virus-caused liver inflammation which may cause jaundice, fever and cirrhosis. Persons who are most at risk for contracting and spreading hepatitis C are those who share needles for injecting drugs and health care workers or emergency workers who may be exposed to contaminated blood.
Hepatitis C
illustration
-
Digestive system - illustration
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
Digestive system
illustration
-
Hepatitis C - illustration
Hepatitis C is a virus-caused liver inflammation which may cause jaundice, fever and cirrhosis. Persons who are most at risk for contracting and spreading hepatitis C are those who share needles for injecting drugs and health care workers or emergency workers who may be exposed to contaminated blood.
Hepatitis C
illustration
Review Date: 1/28/2016
Reviewed By: Subodh K. Lal, MD, gastroenterologist at Gastrointestinal Specialists of Georgia, Austell, GA. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.