Cervical cancer
Cancer - cervix; Cervical cancer - HPV; Cervical cancer - dysplasia
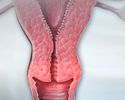
Cervical cancer is cancer that starts in the cervix. The cervix is the lower part of the uterus (womb) that opens at the top of the vagina.
Causes
Worldwide, cervical cancer is the third most common type of cancer in women. It is much less common in the United States because of the routine use of Pap smears .
Pap smears
The Pap test checks for cervical cancer. Cells scraped from the opening of the cervix are examined under a microscope. The cervix is the lower part...

Cervical cancer starts in the cells on the surface of the cervix. There are 2 types of cells on the surface of the cervix, squamous and columnar. Most cervical cancers are from squamous cells.
Cervical cancer usually develops slowly. It starts as a precancerous condition called dysplasia . This condition can be detected by a Pap smear and is 100% treatable. It can take years for dysplasia to develop into cervical cancer. Most women who are diagnosed with cervical cancer today have not had regular Pap smears, or they have not followed up on abnormal Pap smear results.
Dysplasia
Cervical dysplasia refers to abnormal changes in the cells on the surface of the cervix. The cervix is the lower part of the uterus (womb) that open...

Almost all cervical cancers are caused by HPV (human papillomavirus). HPV is a common virus that is spread through sexual intercourse. There are many different types (strains) of HPV. Some strains lead to cervical cancer. Other strains can cause genital warts . Others do not cause any problems at all.
Genital warts
Genital warts are soft growths on the skin and mucus membranes of the genitals. They may be found on the penis, vulva, urethra, vagina, cervix, and ...

A woman's sexual habits and patterns can increase her risk of developing cervical cancer. Risky sexual practices include:
- Having sex at an early age
- Having multiple sexual partners
- Having a partner or many partners who take part in high-risk sexual activities
Other risk factors for cervical cancer include:
-
Not getting the
HPV vaccine
HPV vaccine
The human papillomavirus (HPV) vaccine protects against infection by certain strains of HPV. Human papillomavirus can cause cervical cancer and geni...
Read Article Now Book Mark Article - Being economically disadvantaged
- Having a mother who took the drug diethylstilbestrol (DES) during pregnancy in the early 1960s to prevent miscarriage
- Having a weakened immune system
Symptoms
Most of the time, early cervical cancer has no symptoms. Symptoms that may occur include:
- Abnormal vaginal bleeding between periods, after intercourse, or after menopause
- Vaginal discharge that does not stop, and may be pale, watery, pink, brown, bloody, or foul-smelling
- Periods that become heavier and last longer than usual
Cervical cancer may spread to the bladder, intestines, lungs, and liver. Often, there are no problems until the cancer is advanced and has spread. Symptoms of advanced cervical cancer may include:
- Back pain
- Bone pain or fractures
- Fatigue
- Leaking of urine or feces from the vagina
- Leg pain
- Loss of appetite
- Pelvic pain
- Single swollen leg
- Weight loss
Exams and Tests
Precancerous changes of the cervix and cervical cancer cannot be seen with the naked eye. Special tests and tools are needed to spot such conditions:
- A Pap smear screens for precancers and cancer, but does not make a final diagnosis.
-
The
human papillomavirus (HPV) DNA test
may be done along with a Pap test. Or it may be used after a woman has had an abnormal Pap test result. It may also be used as the first test.
Human papillomavirus (HPV) DNA test
The HPV DNA test is used to check for high-risk HPV infection in women. HPV infection around the genitals is common. It can be spread during sex. ...
Read Article Now Book Mark Article -
If abnormal changes are found, the cervix is usually examined under magnification. This procedure is called
colposcopy
. Pieces of tissue are removed (biopsied) during this procedure. This tissue is then sent to a lab for examination.
Colposcopy
A colposcopy is a special way of looking at the cervix. It uses a light and a low-powered microscope to make the cervix appear much larger. This he...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
A procedure called a
cone biopsy
may also be done.
Cone biopsy
A cold knife cone biopsy (conization) is surgery to remove a sample of abnormal tissue from the cervix. The cervix is the lower part of the uterus (...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
If cervical cancer is diagnosed, the health care provider will order more tests. These help determine how far the cancer has spread. This is called staging. Tests may include:
- Chest x-ray
-
CT scan of the pelvis
CT scan of the pelvis
A computed tomography (CT) scan of the pelvis is an imaging method that uses x-rays to create cross-sectional pictures of the area between the hip bo...
Read Article Now Book Mark Article -
Cystoscopy
Cystoscopy
Cystoscopy is a surgical procedure. This is performed to see the inside of the bladder and urethra using a telescope.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Intravenous pyelogram (IVP)
Intravenous pyelogram (IVP)
An intravenous pyelogram (IVP) is a special x-ray exam of the kidneys, bladder, and ureters (the tubes that carry urine from the kidneys to the bladd...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
MRI of the pelvis
MRI of the pelvis
A pelvis MRI (magnetic resonance imaging) scan is a imaging test that uses a machine with powerful magnets and radio waves to create pictures of the ...
Read Article Now Book Mark Article
Treatment
Treatment of cervical cancer depends on:
- The stage of the cancer
- The size and shape of the tumor
- The woman's age and general health
- Her desire to have children in the future
Early cervical cancer can be cured by removing or destroying the precancerous or cancerous tissue. This is why routine Pap smears are so important to prevent cervical cancer. There are surgical ways to do this without removing the uterus or damaging the cervix, so that a woman can still have children in the future.
Types of surgery for early cervical cancer include:
- Loop electrosurgical excision procedure (LEEP): Uses electricity to remove abnormal tissue
- Cryotherapy: Freezes abnormal cells
- Laser therapy: Uses light to burn abnormal tissue
A hysterectomy (surgery to remove the uterus but not the ovaries) is not often done for cervical cancer that has not spread. It may be done in women who have had repeated LEEP procedures.
Hysterectomy
Hysterectomy is surgery to remove a woman's womb (uterus). The uterus is a hollow muscular organ that nourishes the developing baby during pregnancy...

Treatment for more advanced cervical cancer may include:
- Radical hysterectomy, which removes the uterus and much of the surrounding tissues, including lymph nodes and the upper part of the vagina.
- Pelvic exenteration, an extreme type of surgery in which all of the organs of the pelvis, including the bladder and rectum, are removed.
Radiation may be used to treat cancer that has spread beyond the cervix or cancer that has returned.
Radiation
Radiation therapy uses high-powered x-rays, particles, or radioactive seeds to kill cancer cells.

Chemotherapy uses drugs to kill cancer. It may be given alone or with surgery or radiation.
Chemotherapy
The term chemotherapy is used to describe cancer-killing drugs. Chemotherapy may be used to:Cure the cancerShrink the cancerPrevent the cancer from ...

Support Groups
You can ease the stress of illness by joining a cancer support group . Sharing with others who have common experiences and problems can help you not feel alone.
Cancer support group
The following organizations are good resources for information on cancer:American Cancer Society -- www. cancer. orgCancerCare -- www. cancercare. or...
Outlook (Prognosis)
How well the person does depends on many things, including:
- Type of cervical cancer
- Stage of cancer (how far it has spread)
- Age and general health
- If the cancer comes back after treatment
Precancerous conditions can be completely cured when followed up and treated properly. Most women are alive in 5 years (5-year survival rate) for cancer that has spread to the inside of the cervix walls but not outside the cervix area. The 5-year survival rate falls as the cancer spreads outside the walls of the cervix into other areas.
Possible Complications
Complications can include:
- Risk of the cancer coming back in women who have treatment to save the uterus
- Problems with sexual, bowel, and bladder function after surgery or radiation
When to Contact a Medical Professional
Call your provider if you:
- Have not had regular Pap smears
- Have abnormal vaginal bleeding or discharge
Prevention
Cervical cancer can be prevented by doing the following:
-
Get the
HPV vaccine
. The vaccine prevents most types of HPV infection that cause cervical cancer. Your provider can tell you if the vaccine is right for you.
HPV vaccine
The human papillomavirus (HPV) vaccine protects against infection by certain strains of HPV. Human papillomavirus can cause cervical cancer and geni...
Read Article Now Book Mark Article - Practice safer sex. Using condoms during sex reduces the risk for HPV and other sexually transmitted infections (STIs).
- Limit the number of sexual partners you have. Avoid partners who are active in high-risk sexual behaviors.
- Get Pap smears as often as your provider recommends. Pap smears can help detect early changes, which can be treated before they turn into cervical cancer.
- Get the HPV test if recommended by your provider. It can be used along with the Pap test to screen for cervical cancer in women 30 years and older.
-
If you smoke, quit
. Smoking increases your chance of getting cervical cancer.
If you smoke, quit
If you smoke, you should quit. But quitting can be hard. Most people who have quit smoking have tried at least once, without success, in the past. ...
Read Article Now Book Mark Article
References
Committee on Adolescent Health Care of the American College of Obstetricians and Gynecologists: Immunization Expert Work Group of the American College of Obstetricians and Gynecologists. Committee Opinion No. 588: human papillomavirus vaccination. Obstet Gynecol . 2014;123:712-718. PMID: 24553168 www.ncbi.nlm.nih.gov/pubmed/24553168 .
Hacker NF. Cervical dysplasia and cancer. In: Hacker NF, Gambone JC, Hobel CJ, eds. Hacker and Moore's Essentials of Obstetrics and Gynecology . 6th ed. Philadelphia, PA: Elsevier; 2016:chap 38.
Jhingran A, Russell AH, Seiden MV, et al. Cancers of the cervix, vulva, and vagina. In: Niederhuber JE, Armitage JO, Doroshow JH, Kastan MB, Tepper JE, eds. Abeloff's Clinical Oncology . 5th ed. Philadelphia, PA: Elsevier; 2013:chap 87.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology (NCCN guidelines): cervical cancer. Version 1.2016. www.nccn.org/professionals/physician_gls/pdf/cervical.pdf . Accessed: January 18, 2016.
U.S. Preventive Services Task Force. Screening for Cervical Cancer: U.S. Preventive Services Task Force recommendation statement. AHRQ Publication No. 11-05156-EF-2, March 2012. www.uspreventiveservicestaskforce.org/uspstf11/cervcancer/cervcancerrs.htm . Accessed: January 18, 2016.
-
Cervical cancer
Animation
-
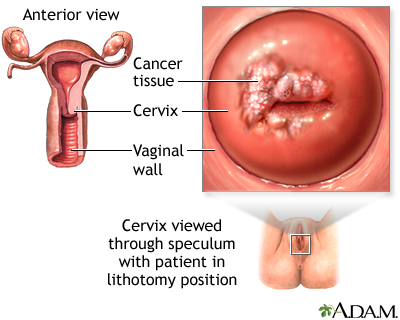
Cervical cancer - illustration
The development of cervical cancer is gradual and begins as a pre-cancerous condition called dysplasia. It is usually a slow-growing cancer and if caught early can be successfully treated. Routine Pap smears can detect early changes in the cells of the cervix allowing cervical cancer to be caught early.
Cervical cancer
illustration
-
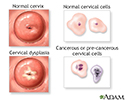
Cervical neoplasia - illustration
Cervical intraepithelial neoplasia (CIN) is the presence of abnormal cells on the surface of the cervix. A Pap smear and colposcopy are two of the procedures performed to monitor the cells and appearance of the cervix.
Cervical neoplasia
illustration
-
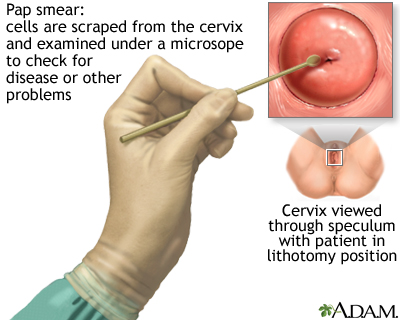
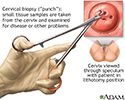
Pap smear - illustration
A Pap test is a simple, relatively inexpensive procedure that can easily detect cancerous or precancerous conditions.
Pap smear
illustration
-
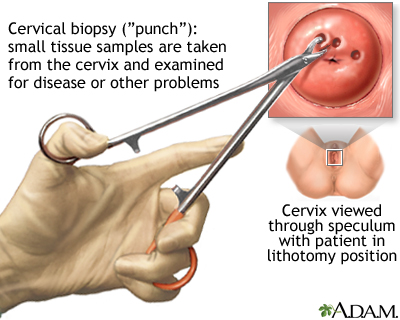
Cervical biopsy - illustration
In a cervical punch biopsy, the cervix may be stained with iodine solution in order to see abnormalities better. These areas of tissue are then sampled and examined.
Cervical biopsy
illustration
-
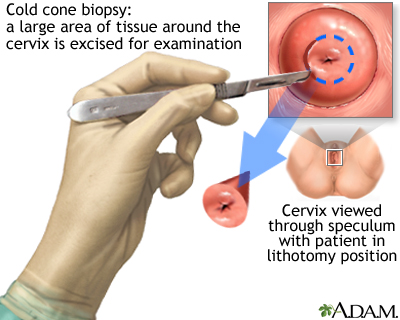
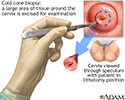
Cold cone biopsy - illustration
The cold cone biopsy is a surgical procedure requiring general anesthesia and is indicated by the presence of precancerous changes in the cervix.
Cold cone biopsy
illustration
-
Cervical cancer - illustration
Cervical cancer is the third most common type of cancer in women. Approximately 2-3% of all women over age 40 years will develop some form of cervical cancer.
Cervical cancer
illustration
-
Pap smears and cervical cancer - illustration
An instrument called a speculum holds the walls of the vagina open so that the cervix may be viewed and a swab of cells obtained for analysis.
Pap smears and cervical cancer
illustration
-
Cervical cancer - illustration
The development of cervical cancer is gradual and begins as a pre-cancerous condition called dysplasia. It is usually a slow-growing cancer and if caught early can be successfully treated. Routine Pap smears can detect early changes in the cells of the cervix allowing cervical cancer to be caught early.
Cervical cancer
illustration
-
Cervical neoplasia - illustration
Cervical intraepithelial neoplasia (CIN) is the presence of abnormal cells on the surface of the cervix. A Pap smear and colposcopy are two of the procedures performed to monitor the cells and appearance of the cervix.
Cervical neoplasia
illustration
-
Pap smear - illustration
A Pap test is a simple, relatively inexpensive procedure that can easily detect cancerous or precancerous conditions.
Pap smear
illustration
-
Cervical biopsy - illustration
In a cervical punch biopsy, the cervix may be stained with iodine solution in order to see abnormalities better. These areas of tissue are then sampled and examined.
Cervical biopsy
illustration
-
Cold cone biopsy - illustration
The cold cone biopsy is a surgical procedure requiring general anesthesia and is indicated by the presence of precancerous changes in the cervix.
Cold cone biopsy
illustration
-
Cervical cancer - illustration
Cervical cancer is the third most common type of cancer in women. Approximately 2-3% of all women over age 40 years will develop some form of cervical cancer.
Cervical cancer
illustration
-
Pap smears and cervical cancer - illustration
An instrument called a speculum holds the walls of the vagina open so that the cervix may be viewed and a swab of cells obtained for analysis.
Pap smears and cervical cancer
illustration
-
Cervical dysplasia
(Alt. Medicine)
Review Date: 12/4/2015
Reviewed By: Yi-Bin Chen, MD, Leukemia/Bone Marrow Transplant Program, Massachusetts General Hospital, Boston, MA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.