Epilepsy - overview
Seizure disorder; Epileptic - epilepsy
Epilepsy is a brain disorder in which a person has repeated seizures over time. Seizures are episodes of uncontrolled and abnormal firing of brain cells that may cause changes in attention or behavior.
Seizures
A seizure is the physical findings or changes in behavior that occur after an episode of abnormal electrical activity in the brain. The term "seizure...

Causes
Epilepsy occurs when permanent changes in the brain cause it to be too excitable or irritable. As a result, the brain sends out abnormal signals. This leads to repeated, unpredictable seizures. (A single seizure that does not happen again is not epilepsy.)
Epilepsy may be due to a medical condition or injury that affects the brain. Or the cause may be unknown (idiopathic).
Common causes of epilepsy include:
-
Stroke
or transient ischemic attack (
TIA
)
Stroke
A stroke occurs when blood flow to a part of the brain stops. A stroke is sometimes called a "brain attack. " If blood flow is cut off for longer th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleTIA
A transient ischemic attack occurs when blood flow to a part of the brain stops for a brief time. A person will have stroke-like symptoms for up to ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Dementia
, such as Alzheimer disease
Dementia
Dementia is a loss of brain function that occurs with certain diseases. It affects memory, thinking, language, judgment, and behavior.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Traumatic brain injury
-
Infections, including
brain abscess
,
meningitis
,
encephalitis
, and
HIV/AIDS
Brain abscess
A brain abscess is a collection of pus, immune cells, and other material in the brain, usually from a bacterial or fungal infection.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleMeningitis
Meningitis is an infection of the membranes covering the brain and spinal cord. This covering is called the meninges.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleEncephalitis
Encephalitis is irritation and swelling (inflammation) of the brain, most often due to infections.
Read Article Now Book Mark ArticleHIV/AIDS
Human immunodeficiency virus (HIV) is the virus that causes AIDS. When a person becomes infected with HIV, the virus attacks and weakens the immune ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Brain problems that are present at birth (congenital brain defect)
- Brain injury that occurs during or near birth
-
Metabolism disorders present at birth (such as
phenylketonuria
)
Phenylketonuria
Phenylketonuria (PKU) is a rare condition in which a baby is born without the ability to properly break down an amino acid called phenylalanine....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Brain tumor
- Abnormal blood vessels in the brain
- Other illness that damages or destroys brain tissue
Epileptic seizures usually begin between ages 5 and 20. There is also a higher chance of seizures in adults older than 60. But epileptic seizures can happen at any age. There may be a family history of seizures or epilepsy.
Symptoms
Symptoms vary from person to person. Some people may have simple staring spells. Others have violent shaking and loss of alertness. The type of seizure depends on the part of the brain that is affected.
Most of the time, the seizure is similar to the one before it. Some people with epilepsy have a strange sensation before each seizure. Sensations may be tingling, smelling an odor that is not actually there, or emotional changes. This is called an aura.
Your doctor can tell you more about the specific type of seizure you may have:
-
Absence (petit mal) seizure
(staring spells)
Absence (petit mal) seizure
An absence seizure is the term for a type of seizure involving staring spells. This type of seizure is a brief (usually less than 15 seconds) distur...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Generalized tonic-clonic (grand mal) seizure
(involves the entire body, including aura, rigid muscles, and loss of alertness)
Generalized tonic-clonic (grand mal) se...
Generalized tonic-clonic seizure is 1 type of seizure that involves the entire body. It is also called grand mal seizure. The terms seizure, convul...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Partial (focal) seizure
(can involve any of the symptoms described above, depending on where in the brain the seizure starts)
Partial (focal) seizure
All seizures are caused by abnormal electrical disturbances in the brain. Partial (focal) seizures occur when this electrical activity remains in a ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Exams and Tests
The doctor will perform a physical exam. This will include a detailed look at the brain and nervous system.
An EEG (electroencephalogram) will be done to check the electrical activity in the brain. People with epilepsy often have abnormal electrical activity seen on this test. In some cases, the test shows the area in the brain where the seizures start. The brain may appear normal after a seizure or between seizures.
EEG
An electroencephalogram is a test to measure the electrical activity of the brain.

To diagnose epilepsy or plan for epilepsy surgery, you may need to:
- Wear an EEG recorder for days or weeks as you go about your everyday life.
- Stay in a special hospital where brain activity can be recorded while video cameras capture what happens to you during the seizure. This is called video EEG.
Tests that may be done include:
- Blood chemistry
-
Blood sugar
Blood sugar
A blood glucose test measures the amount of a sugar called glucose in a sample of your blood. Glucose is a major source of energy for most cells of t...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Complete blood count (
CBC
)
CBC
A complete blood count (CBC) test measures the following:The number of red blood cells (RBC count)The number of white blood cells (WBC count)The tota...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Kidney function tests
Kidney function tests
Kidney function tests are common lab tests used to evaluate how well the kidneys are working. Such tests include:BUN (Blood urea nitrogen) Creatinin...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Liver function tests
Liver function tests
Liver function tests are common tests that are used to see how well the liver is working. Tests include:AlbuminAlpha-1 antitrypsin Alkaline phosph...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Lumbar puncture
(spinal tap)
Lumbar puncture
Cerebrospinal fluid (CSF) collection is a test to look at the fluid that surrounds the brain and spinal cord. CSF acts as a cushion, protecting the b...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Tests for infectious diseases
Head CT or MRI scan is often done to find the cause and location of the problem in the brain.
CT
A head computed tomography (CT) scan uses many x-rays to create pictures of the head, including the skull, brain, eye sockets, and sinuses.

MRI
A head MRI (magnetic resonance imaging) is an imaging test that uses powerful magnets and radio waves to create pictures of the brain and surrounding...

Treatment
Treatment for epilepsy includes taking medicines, lifestyle changes, and sometimes surgery.
If epilepsy is due to a tumor, abnormal blood vessels, or bleeding in the brain, surgery to treat these disorders may make the seizures stop.
Medicines to prevent seizures, called anticonvulsants (or antiepileptic drugs), may reduce the number of future seizures:
- These drugs are taken by mouth. Which type you are prescribed depends on the type of seizures you have.
- Your dosage may need to be changed from time to time. You may need regular blood tests to check for side effects.
- Always take your medicine on time and as directed. Missing a dose can cause you to have a seizure. DO NOT stop taking or change medicines on your own. Talk to your doctor first.
- Many epilepsy medicines cause birth defects. Women who plan to become pregnant should tell their doctor in advance in order to adjust medicines.
Many epilepsy drugs may affect the health of your bones. Talk to your doctor about whether you need vitamins and other supplements.
Epilepsy that does not get better after 2 or 3 anti-seizure drugs have been tried is called "medically refractory epilepsy." In this case, the doctor may recommend surgery to:
- Remove the abnormal brain cells causing the seizures.
- Place a vagal nerve stimulator (VNS). This device is similar to a heart pacemaker. It can help reduce the number of seizures.
Some children are placed on a special diet to help prevent seizures. The most popular one is the ketogenic diet. A diet low in carbohydrates, such as the Atkins diet, may also be helpful in some adults. Be sure to discuss these options with your doctor before trying them.
Lifestyle or medical changes can increase the risk for a seizure in adults and children with epilepsy. Talk with your doctor about:
Adults
You have epilepsy. People with epilepsy have seizures. A seizure is a sudden brief change in the electrical and chemical activity in the brain. Th...
- New prescribed drugs, vitamins, or supplements
- Emotional stress
- Illness, especially infection
- Lack of sleep
- Pregnancy
- Skipping doses of epilepsy medicines
- Use of alcohol or other recreational drugs
Other considerations:
- People with epilepsy should wear medical alert jewelry so that prompt treatment can be obtained if a seizure occurs.
- People with poorly controlled epilepsy should not drive. Check your state's law about which people with a history of seizures are allowed to drive.
- DO NOT use machinery or do activities that can cause loss of awareness, such as climbing to high places, biking, and swimming alone.
Support Groups
The stress of having epilepsy or being a caretaker of someone with epilepsy can often be helped by joining a support group . In these groups, members share common experiences and problems.
Support group
The following organizations are good resources for information on epilepsy:Epilepsy Foundation -- www. epilepsy. comNational Institute of Neurologica...

Outlook (Prognosis)
Some people with epilepsy may be able to reduce or even stop their anti-seizure medicines after having no seizures for several years. Certain types of childhood epilepsy go away or improve with age, usually in the late teens or 20s.
For many people, epilepsy is a lifelong condition. In these cases, anti-seizure drugs need to be continued. There is a very low risk for sudden death with epilepsy.
Possible Complications
Complications may include:
- Difficulty learning
- Breathing in food or saliva into the lungs during a seizure, which can cause aspiration pneumonia
- Injury from falls, bumps, self-inflicted bites, driving or operating machinery during a seizure
- Permanent brain damage (stroke or other damage)
- Side effects of medicines
When to Contact a Medical Professional
Call your local emergency number (such as 911) if:
- This is the first time a person has a seizure
- A seizure occurs in someone who is not wearing a medical ID bracelet (which has instructions explaining what to do)
In the case of someone who has had seizures before, call 911 for any of these emergency situations:
- This is a longer seizure than the person normally has, or an unusual number of seizures for the person
- Repeated seizures over a few minutes
- Repeated seizures in which consciousness or normal behavior is not regained between them (status epilepticus)
Call your doctor if any new symptoms occur:
- Loss of hair
- Nausea or vomiting
- Rash
- Side effects of medicines, such as drowsiness, restlessness, confusion, sedation
- Tremors or abnormal movements, or problems with coordination
Prevention
There is no known way to prevent epilepsy. Proper diet and sleep, and staying away from alcohol and illegal drugs may decrease the likelihood of triggering seizures in people with epilepsy.
Reduce the risk for head injury by wearing a helmet during risky activities. This can lessen the likelihood of a brain injury that leads to seizures and epilepsy.
References
Abou-Khalil BW, Gallagher MJ, Macdonald RL. Epilepsies. In: Daroff RB, Jankovic J, Mazziotta JC, Pomeroy SK, eds. Bradley's Neurology in Clinical Practice . 7th ed. Philadelphia, PA: Elsevier; 2016:chap 101.
Morris GL III, Gloss D, Buchhalter J, Mack KJ, Nickels K, Harden C. Evidence-based guideline update: vagus nerve stimulation for the treatment of epilepsy: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology . 2013;81:1453-1459. PMID: 23986299 www.ncbi.nlm.nih.gov/pubmed/23986299 .
Wiebe S. The epilepsies. In: Goldman L, Schafer AI, eds. Goldman's Cecil Medicine . 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 403.
-
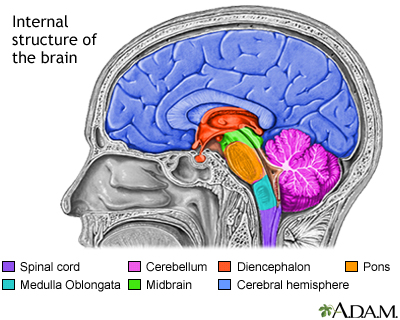
Brain structures - illustration
The structures of the brain include: the brainstem, consisting of the spinal cord, the medulla oblongata, the pons and the midbrain; the cerebellum; the cerebrum (one half, or hemisphere shown), and the diencephalon .
Brain structures
illustration
-
Limbic system - illustration
The limbic system of the brain is a group of structures which govern emotions and behavior. The limbic system, and in particular the hippocampus and amygdala, is involved in the formation of long-term memory, and is closely associated with the olfactory structures (having to do with the sense of smell).
Limbic system
illustration
-
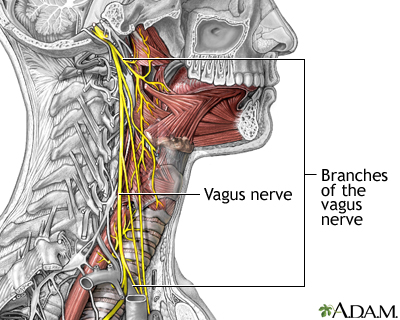
Role of the vegus nerve in epilepsy - illustration
The vagus nerves branch off the brain on either side of the head and travel down the neck, along the esophagus to the intestinal tract. They are the longest nerves in the body, and affect swallowing and speech. The vagus nerves also connect to parts of the brain involved in seizures. In many seizures disorders, electrical stimulation of the vagus nerves may afford relief of symptoms.
Role of the vegus nerve in epilepsy
illustration
-
Central nervous system and peripheral nervous system - illustration
The central nervous system is comprised of the brain and spinal cord. The peripheral nervous system includes all peripheral nerves.
Central nervous system and peripheral nervous system
illustration
-
Brain structures - illustration
The structures of the brain include: the brainstem, consisting of the spinal cord, the medulla oblongata, the pons and the midbrain; the cerebellum; the cerebrum (one half, or hemisphere shown), and the diencephalon .
Brain structures
illustration
-
Limbic system - illustration
The limbic system of the brain is a group of structures which govern emotions and behavior. The limbic system, and in particular the hippocampus and amygdala, is involved in the formation of long-term memory, and is closely associated with the olfactory structures (having to do with the sense of smell).
Limbic system
illustration
-
Role of the vegus nerve in epilepsy - illustration
The vagus nerves branch off the brain on either side of the head and travel down the neck, along the esophagus to the intestinal tract. They are the longest nerves in the body, and affect swallowing and speech. The vagus nerves also connect to parts of the brain involved in seizures. In many seizures disorders, electrical stimulation of the vagus nerves may afford relief of symptoms.
Role of the vegus nerve in epilepsy
illustration
-
Central nervous system and peripheral nervous system - illustration
The central nervous system is comprised of the brain and spinal cord. The peripheral nervous system includes all peripheral nerves.
Central nervous system and peripheral nervous system
illustration
Review Date: 2/27/2016
Reviewed By: Amit M. Shelat, DO, FACP, Attending Neurologist and Assistant Professor of Clinical Neurology, SUNY Stony Brook, School of Medicine, Stony Brook, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.