Epilepsy
An in-depth report on the types, causes, diagnosis, and treatment of epilepsy.
Highlights
Epilepsy is a brain disorder that is marked by recurrent seizures. Seizures are episodes of disturbed brain function caused by abnormalities of the brain's electrical activity. There are many types of seizures.
CausesEpilepsy can affect people of all ages but is most common in young children and older adults. Some types of epilepsy are inherited and are due to genetic factors. Other possible causes of epilepsy include brain injuries due to head trauma or oxygen deprivation at birth. In many cases, the cause of epilepsy is unknown (idiopathic).
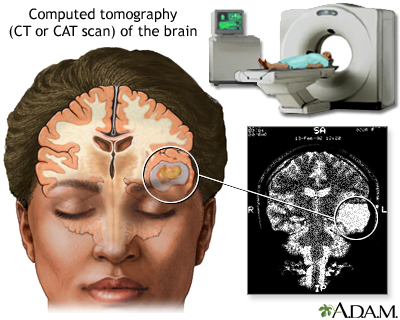
DiagnosisA health care provider will diagnose epilepsy based on a person's medical history, description of seizures, and various diagnostic tools. The most important diagnostic tool is the electroencephalogram (EEG), which allows providers to record and analyze brain waves. Imaging tests such as computed tomography (CT) and magnetic resonance imaging (MRI) may also be used.
TreatmentThe goal of epilepsy treatment is to control seizures. Many different types of anticonvulsant (anti-epileptic) drugs are available to treat epilepsy. Some people need only one drug, while others may need to take several drugs.
For people who have not been helped by medication, surgery or a neurostimulation device may be options. Dietary changes, such as the ketogenic diet, have shown promise in helping children with severe epilepsy.
Anti-epileptic drugs (AEDs) can cause many side effects. Pregnant women with epilepsy need to take special precautions, because some of these drugs (particularly valproate) can cause birth defects.
Introduction
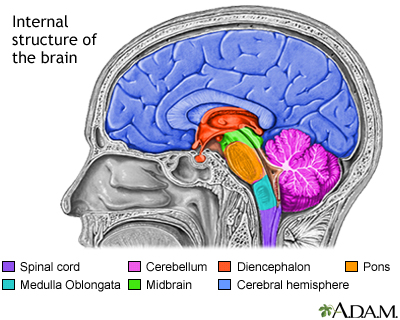
Epilepsy is a brain disorder involving repeated, spontaneous seizures of any type. There are different types of epilepsy but what they all share are recurrent seizures caused by an uncontrolled electrical discharge from nerve cells in the cerebral cortex. This part of the brain controls higher mental functions, general movement and sensation, the functions of the internal organs in the abdominal cavity, perception, and behavioral reactions.
The structures of the brain include the brainstem, consisting of the spinal cord, the medulla oblongata, the pons and the midbrain; the cerebellum; the cerebrum (one half, or hemisphere shown); and the diencephalon.
Seizures
Seizures are a symptom of epilepsy. Seizures are episodes of disturbed brain function that cause changes in neuromuscular function, attention, or behavior. They are caused by abnormally excited electrical signals in the brain.
Seizures can also be caused by conditions other than epilepsy. Many people experience a single seizure at some point in their life and then never experience another. A single seizure may be related to a specific medical problem such as fever, a reaction to a drug, or withdrawal from alcohol. This situation is different from epilepsy.
Epilepsy is a condition that causes permanent changes in the brain and disturbs how electrical energy works in the brain. The seizures that are associated with epilepsy are provoked by abnormal bursts of electrical activity in the brain.
Types of Epilepsy
Epilepsy is generally classified into two main categories based on seizure type:
- Partial (also called focal or localized) seizures: Partial seizures are more common than generalized seizures and occur in one or more specific locations in the brain. In some cases, partial seizures can spread to wide regions of the brain. They are likely to develop from specific injuries, but in most cases the exact origins are unknown (idiopathic).
- Generalized seizures: Generalized seizures typically occur in both sides of the brain. Many forms of these seizures are genetically based. People usually have normal neurologic function between episodes.
Partial Seizures (also called Focal Seizures)
Partial (focal) seizures are subcategorized as "simple" or "complex partial":
- Simple Partial Seizures. A person with a simple partial seizure (sometimes known as Jacksonian epilepsy) does not lose consciousness, but may experience confusion, jerking movements (convulsions), tingling, or odd mental and emotional events. Such events may include déjà vu, mild hallucinations, or extreme responses to smell and taste. After the seizure, there is usually temporary muscular weakness. These seizures typically last about 90 seconds.
- Complex Partial Seizures. Slightly over half of all seizures in adults are complex partial type. About 80% of these seizures originate in the temporal lobe, the part of the brain located close to the ear. Temporal lobe disturbances can result in loss of judgment, involuntary or uncontrolled behavior, or loss of consciousness. People may lose consciousness briefly and appear to others as motionless with a vacant stare. Emotions can be exaggerated; some people even appear to be drunk. After a few seconds, a person may begin to perform repetitive movements, such as chewing or smacking of lips. Episodes usually last no more than 2 minutes. They may occur infrequently, or as often as every day. A throbbing headache may follow a complex partial seizure.
Generalized Seizures
Generalized seizures are caused by nerve cell disturbances that occur in more widespread areas of the brain than partial seizures. Therefore, they have more serious effects. They are further subcategorized as tonic-clonic (or grand mal), absence (petit mal), myoclonic, or atonic seizures.
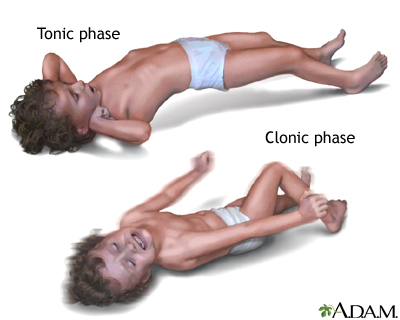
Tonic-Clonic (Grand Mal) Seizures: The first stage of a grand mal seizure is called the tonic phase. The muscles suddenly contract, causing the person to fall and lie stiffly for about 10 to 30 seconds. Some people experience a premonition or aura before a grand mal seizure. Most, however, lose consciousness without warning. If the throat or larynx is affected, there may be a high-pitched musical sound (stridor) when the person inhales.Spasms occur for about 30 seconds to 1 minute. The seizure then enters the second phase, called the clonic phase. The muscles begin to alternate between relaxation and rigidity. Loss of bowel or urinary control may occur. The seizure usually lasts a total of 2 to 3 minutes. The person remains unconscious for a while and then awakens to confusion and extreme fatigue. A severe throbbing headache similar to migraine may also follow the tonic-clonic phases.
Absence (Petit Mal) Seizures: Absence or petit mal seizures are brief losses of consciousness that occur for 3 to 30 seconds. Physical activity and loss of attention may pause for only a moment. Such seizures may pass unnoticed by others. Young children may simply appear to be staring or walking distractedly. Petit mal may be confused with simple or complex partial seizures, or even with attention deficit hyperactivity disorder (ADHD). In petit mal, however, a person may experience attacks as often as 50 to 100 times a day. Myoclonic Seizures: Myoclonic seizures are a series of brief jerky contractions of specific muscle groups, such as the face or trunk. Atonic (Akinetic) Seizures: A person who has an atonic (or akinetic) seizure loses muscle tone. Sometimes it may affect only one part of the body so that, for instance, the jaw slackens and the head drops. At other times, the whole body may lose muscle tone, and the person can suddenly fall. A brief atonic episode is known as a drop attack. Simply Tonic or Clonic Seizures: Seizures can also be simply tonic or clonic. In tonic seizures, the muscles contract and consciousness is altered for about 10 seconds, but the seizures do not progress to the clonic or jerking phase. Clonic seizures, which are very rare, occur primarily in young children, who experience spasms of the muscles but not tonic rigidity.Epilepsy Syndromes
Epilepsy is also grouped according to a set of common characteristics, including:
- Age
- Type of seizure or seizures
- Behavior during seizure
- Results of EEG recordings
- Whether a cause is known or not known (idiopathic)
A few syndromes and inherited epilepsies are listed below. They do not represent all epilepsies.
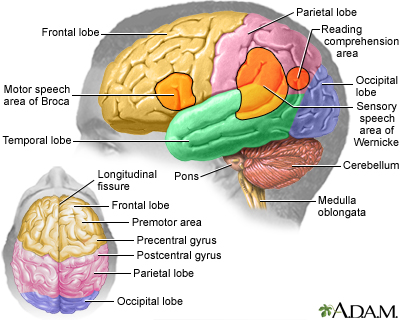
Temporal Lobe Epilepsy: Temporal lobe epilepsy is a form of partial (focal) epilepsy, although generalized tonic-clonic seizures may occur with it. Frontal Lobe Epilepsy: Frontal lobe epilepsy is characterized by sudden violent seizures. Seizures may also produce loss of muscle function, including the ability to talk. In autosomal dominant nocturnal frontal lobe epilepsy, a rare inherited form, seizures often occur during sleep. West Syndrome (Infantile Spasms): West syndrome, also called infantile spasms, is a disorder that involves spasms and developmental delay in children within the first year, usually in infants ages 4 to 8 months. Benign Familial Neonatal Convulsions: Benign familial neonatal convulsions (BFNC) are a rare, inherited form of generalized seizures that occur in infancy. BFNC appears to be caused by genetic defects that affect channels in nerve cells that carry potassium. Juvenile Myoclonic Epilepsy (Impulsive Petit Mal): Juvenile myoclonic epilepsy, also called impulsive petit mal epilepsy, is characterized by generalized seizures, usually tonic-clonic marked by jerky movements (called myoclonic jerks), and sometimes absence seizures. It usually occurs in younger people ages 8 to 20. Lennox-Gastaut Syndrome: Lennox-Gastaut syndrome is a severe form of epilepsy in young children that causes multiple seizures and some developmental disability. It usually involves absence, tonic, and partial seizures. Myoclonic-Astatic Epilepsy: Myoclonic-astatic epilepsy (MAE) is a combination of myoclonic seizures and astasia (a decrease or loss of muscular coordination), often resulting in the inability to sit or stand without aid. Progressive Myoclonic Epilepsy: Progressive myoclonic epilepsy is a rare inherited disorder typically occurring in children ages 6 to 15. It usually involves tonic-clonic seizures and marked sensitivity to light flashes. Landau-Kleffner Syndrome: Landau-Kleffner syndrome is a rare epileptic condition that typically affects children ages 3 to 7. It results in the loss of ability to communicate either with speech or by writing (aphasia).Seizures That Are Not Epilepsy
Non-Epileptic Seizures: Non-epileptic seizures refer to events that resemble epileptic seizures but are not caused by abnormal electrical activity in the brain. Non-epileptic seizures may be physical or psychological in origin.Physiologic non-epileptic seizures result from conditions such as sudden drops in blood pressure (syncope), abnormal heart rhythms (cardiac arrhythmia), low blood sugar associated with diabetes (hypoglycemia), or sleep disorders such as narcolepsy. Psychogenic non-epileptic seizures are usually due to emotional trauma or stress.
Febrile Seizures: Febrile seizures are convulsions in children triggered by a high fever. Most febrile seizures occur in young children ages 9 months to 5 years. Simple febrile seizures last for less than 15 minutes and only occur once in a 24-hour period. They are usually an isolated event and not a sign of underlying epilepsy. However, complex febrile seizures, which last longer than 15 minutes and occur more than once in 24 hours, may be a sign of underlying neurologic problems or epilepsy. Eclampsia: Eclampsia is a life-threatening pregnancy complication associated with tonic-clonic seizures. It can result in pregnant women who develop preeclampsia, a condition marked by extremely high blood pressure and excess fluid in the lungs. First Seizure: A single seizure may be due to causes other than epilepsy (fever, infections, drug reactions, and head trauma). Many people who have a first seizure will never have another seizure, and do not have epilepsy. Still, a health care provider may order a brain imaging test to make sure that epilepsy is not an underlying cause.
Causes
Epileptic seizures are triggered by abnormalities in the brain that cause a group of nerve cells in the cerebral cortex (gray matter) to become activated simultaneously. The activation causes sudden and excessive bursts of electrical energy.
A seizure's effect depends in part on the location in the brain where this electrical hyperactivity occurs. Effects range from brief moments of confusion to minor spasms to loss of consciousness. In most cases of epilepsy, the cause is unknown (idiopathic).
Brain Chemistry Factors
Ion Channels: Sodium, potassium, and calcium act as ions in the brain. They produce electric charges that must fire regularly in order for a steady current to pass from one nerve cell in the brain to another. If the ion channels that carry them are genetically damaged, a chemical imbalance occurs. This can cause nerve signals to misfire, leading to seizures. Neurotransmitters: Abnormalities may occur in neurotransmitters, the chemicals that act as messengers between nerve cells. Three neurotransmitters are of particular importance: Scientists in epilepsy research have paid particular attention to the neurotransmitter gamma aminobutyric acid (GABA), which helps prevent nerve cells from over-firing.Genetic Factors
Some types of epilepsy are inherited conditions where genetics play a factor. Generalized epilepsy seizure types appear to be more related to genetic influences than partial seizure epilepsies.
Brain Damage
Epilepsy can be caused by many types of diseases or injuries that damage the brain. Head trauma can bring on seizures and epilepsy. Cerebral palsy and other disorders caused by lack of oxygen to the brain during birth are often associated with epilepsy.
Epilepsy can also develop from another medical condition that affects the brain or central nervous system. Examples include:
- Brain tumors
- Traumatic brain injury, stroke, or a transient ischemic attack (TIA)
- Infections in the central nervous system (brain abscess, meningitis, encephalitis, neurosyphilis, or AIDS)
- Poisoning caused by prolonged exposure to certain types of chemicals (lead and carbon monoxide)
Risk Factors
Age
Epilepsy affects all age groups but is most common in the very young and the very old. The risk is highest in children under the age of 2 and in older adults over age 65. In infants and toddlers, prenatal factors and birth delivery problems are associated with epilepsy risk.
In children age 10 and younger, generalized seizures are more common. In older children, partial seizures are more common.
Gender
Males have a slightly higher risk than females of developing epilepsy.
Family History
People who have a family history of epilepsy are at increased risk of developing the condition.
Complications
People with epilepsy generally have a normal lifespan. However, they are at risk for health complications.
Accident-Related Injuries
Injuries from falls: Many people with seizures fall, and injuries are common. Although such injuries are usually minor, people with epilepsy have a higher risk for fractures than those without the disorder. Certain medications (phenytoin, carbamazepine) can affect bone hardness or density and increase the risk for fractures. Household accidents: Household environments, such as the kitchen and bathroom, can be dangerous places for children with epilepsy. Parents should take precautions to prevent burning accidents from stoves and other heat sources. Children with epilepsy should never be left alone when bathing. Driving: Due to the high risk for accidents, people with epilepsy who have seizures that are not controlled by medication are legally restricted from driving. In general, to obtain a driver's license, a health care provider must confirm that a person has been seizure-free for a specific number of months. Swimming: People with epilepsy have a much higher risk for drowning than people without this condition. In fact, one study suggested that the drowning risk for people with epilepsy is 15 to 19 times greater than for the general population. People with epilepsy who swim should avoid deep and cloudy water (a clear swimming pool is best), and always swim with a knowledgeable, competent, and experienced companion or at a facility that has a lifeguard on site.Mental Health Complications
Depression and anxiety are common among people with epilepsy. People with epilepsy have a higher risk for suicide, particularly in the first 6 months following diagnosis. The risk for suicide is highest among people who have epilepsy and an accompanying psychiatric condition, such as depression, anxiety disorder, schizophrenia, or chronic alcohol use. All antiepileptic drugs can increase the risk of suicidal thoughts and behavior. [For more information, see Medications section in this report.]
Learning and Memory Problems
Children with epilepsy often experience problems with learning, attention focus, and memory retention. Some of these problems are due to the after-effects of seizures. Medication side effects, including fatigue and drowsiness, can also be contributing factors. Problems with learning and memory can affect school performance, and lead to behavioral issues.
Sexual and Reproductive Health Complications
Effects on sexual function: Some people with epilepsy experience sexual dysfunction, including erectile dysfunction. These problems may be caused by emotional factors, medication side effects, or a result of changes in hormone levels. Effects on reproductive health: A woman's hormonal fluctuation can affect the course of her seizures. Estrogen appears to increase seizure activity, and progesterone reduces it. Antiseizure medications may reduce the effectiveness of oral contraceptives. Pregnancy complications: Epilepsy can pose risks both to a pregnant woman and her fetus. Some types of anti-epileptic drugs should not be taken during the first trimester because they can cause birth defects. Women with epilepsy who are thinking of becoming pregnant should talk to their health care providers in advance to plan changes in their medication regimen.Status Epilepticus
Status epilepticus (SE) is a prolonged seizure that is a serious, potentially life-threatening condition. It is a medical emergency. Permanent brain damage or death can result if the seizure is not treated effectively.
The condition is generally defined as a continuous seizure that lasts for more than 5 minutes. There are two forms of status epilepticus: generalized convulsive, which involve prolonged seizures, and non-convulsive, which affects behavior and consciousness. About 25% of people who experience status epilepticus have pre-existing epilepsy. Most times, this condition occurs in people who do not have epilepsy and who have never had a prior seizure.
In people with epilepsy, status epilepticus is usually caused by failure to take anticonvulsant medications as directed, or by the abrupt withdrawal from certain medications. Other general causes of status epilepticus include alcohol intoxication or withdrawal, infections, fever, metabolic disorders, stroke, brain tumors, and head trauma.
SUDEP
Although relatively rare, there is a risk for sudden unexpected death in people with epilepsy, a syndrome abbreviated as SUDEP. The causes of such events are not fully known, but heart arrhythmias and pauses in breathing (apnea) may be factors in many cases. Your health care provider can explain if you have specific risk factors for SUDEP and what protective measures can be taken.
The best preventive measure is to take your medication as prescribed. Talk with your provider if you have any concerns about medication side effects or dosages. Do not make any changes to your drug regimen without speaking first with your provider.
Prognosis
The prognosis for epilepsy depends on various factors. In general, people whose epilepsy is well-controlled by medications have an excellent prognosis and many experience short- and even long-term remission from seizures.
The outlook is best for people whose epilepsy responds to treatment soon after being diagnosed. The longer a person remains free from seizures, the lower the chance of seizure recurrence. Some people are able to reduce or even stop their anti-seizure medications after having no seizures for several years.
People who tend to have a poorer prognosis include those with chronic, active epilepsy (high frequency of seizures) that does not respond to early treatment. People who have other illnesses in addition to epilepsy (diabetes and heart disease) are also at increased risk for developing other health problems.
Certain types of childhood epilepsy go away or improve with age, usually by the late teens or 20s. The outlook for childhood epilepsy depends in part on the specific epilepsy syndrome. Syndromes such as childhood absence epilepsy have excellent prognosis, with many children outgrowing the syndrome and experiencing remission by their teenage years. Other syndromes, such as juvenile myoclonic epilepsy, can be well-controlled by medication but are likely to be lifelong.
Epilepsy is considered resolved if a person has been seizure-free for 10 years or has not taken antiepileptic medications for 5 years. "Resolved" does not necessarily mean that the epilepsy is cured or in remission. It implies that a person does not have active epilepsy.
Symptoms
Seizure symptoms vary from person to person. They depend on the part of the brain affected and the type of epilepsy a person has. Most of the time, a seizure is similar to the one that preceded it.
Seizures often have a specific set of symptoms before, during, and after the event.
Before a seizure , people may experience certain warning signs called an aura. They may include:- Sense of déjà vu
- Strange tastes and smells
- Feelings of fear, anxiety, or panic
- Nausea or feeling of stomach rising into throat
- Vertigo and dizziness
- Visual symptoms, such as flashing bright lights, spots, or wavy lines
- Loss of awareness or consciousness
- Repetitive movements (lip smacking or picking at clothing)
- Drooling or frothing at the mouth
- Grunting and snorting
- Staring or blinking
- Strange tastes, smells, and sounds
- Visual hallucinations or seeing flashing lights
- Out of body sensation
- Teeth clenching and tongue biting
- Rigidity of body followed by jerking movements (convulsions)
- Slumping and falling
- Loss of bladder or bowel control
- Headache
- Memory loss
- Fatigue and muscle weakness
- Sleepiness
- Confusion
- Loss of bowel or bladder control
Diagnosis
An epilepsy diagnosis is often made during an emergency visit for a seizure. If a person seeks medical help for a previous or suspected seizure, the health care provider will ask about medical history, including seizure events, and conduct a neurological exam.
Diagnostic Tests
Electroencephalogram (EEG): The most important diagnostic tool for epilepsy is an EEG. An EEG records and measures brain waves, which reflect the electrical activity of nerve cells in the brain. The procedure is painless. It uses electrodes applied to the scalp to send signals to a special box. A routine EEG takes about an hour.In some cases, your provider may want you to do an ambulatory EEG using a portable unit that records brain electrical activity from 24 to 72 hours. Another option is video EEG. This test is conducted in a special hospital room where you will be both monitored by EEG and watched by a video camera to evaluate your behavior during a seizure. You will have an IV so that medications can be administered in case of a prolonged seizure.
Other Neuroimaging Tests: A computerized tomography (CT) scan or magnetic resonance imaging (MRI) scan may be ordered for first-time seizures. More advanced imaging tests may be performed for surgery planning and to identify specific areas in the brain associated with seizure activity. These tests include positron emission tomography (PET), single-photon emission computer tomography (SPECT), and magnetoencephalography (MEG).A CT (computed tomography) scan is a much more sensitive imaging technique than x-ray, allowing high definition of both the bony structures and the soft tissues. Clear images of organs such as the brain, muscles, joint structures, veins and arteries, as well as anomalies like tumors and hemorrhages may be obtained with or without the injection of contrasting dye.
Ruling Out Other Conditions
Conditions that may cause symptoms similar to epilepsy include:
- Syncope (fainting), a brief lapse of consciousness, in which blood flow to the brain is temporarily reduced, can mimic epilepsy. It may be misdiagnosed as a seizure. People with syncope do not have the rhythmic contracting and then relaxing of the body's muscles.
- Migraine headaches , particularly migraine with auras, may sometimes be confused with seizures. With epileptic seizure, the preceding aura is often seen as multiple, brightly colored, circular spots, while migraine tends to cause black, white, or colorless lined or zigzag flickering patterns.
- Panic attacks may resemble partial seizures. Symptoms of a panic attack include palpitations, sweating, trembling, sensation of breathlessness, chest pain, feeling of choking, nausea, faintness, chills or flushes, fear of losing control, and fear of dying.
- Narcolepsy , a sleep disorder that causes a sudden loss of muscle tone and excessive daytime sleepiness, can be confused with epilepsy.
Treatment
What To Do When Someone Has a Seizure
If you see someone have a seizure, remain calm and take the following actions:
- Wipe away any excess saliva to prevent obstruction of the airway. Do not put anything in the person's mouth. It is not true that people having seizures will swallow their tongues.
- Turn the person gently on the side. Do not try to hold the person down to prevent shaking.
- Rest the person's head on something flat and soft to protect it from banging on the floor and to support the neck. Loosen clothes to make breathing easier.
- Move sharp objects out of the way to prevent injury.
- Time the seizure with your watch.
- Do not leave the person alone. Stay with them until they are fully awake. Do not offer them any food or water until they are fully conscious.
You should call 911 if:
- The seizure lasts more than 5 minutes or is followed by a second seizure
- The person has been injured
- The person is pregnant or has diabetes or a heart condition
- The person does not wake up after the seizure
Drug Treatment
Epilepsy is treated with anti-epileptic drugs (AEDs). For people with severe epilepsy that has not been helped by drugs, surgery or a neurostimulation device may be options.
AEDs are used to prevent recurrent seizures. Drug therapy is not usually recommended after a single initial seizure, unless imaging tests reveal brain injuries or a diagnosed epilepsy syndrome suggests increased risk for recurrence In general, drug therapy is considered after a person has had 2 or 3 seizures.
Treatment During Pregnancy
Preparing to Become Pregnant: Women with epilepsy who are considering pregnancy should talk to their health care providers before they become pregnant. According to guidelines from the American Academy of Neurology and the American Epilepsy Society:- A woman who has been seizure-free for at least 9 months before becoming pregnant has a good chance of remaining seizure free during pregnancy.
- Folic acid is recommended for all pregnant women. Women with epilepsy should consider taking folic acid supplements at least 3 months before conception as well as during the pregnancy.
- Women with epilepsy do not face a substantially increased risk of premature birth or labor and delivery complications (including cesarean section). However, smoking may increase the risk of premature delivery.
- Babies born to mothers who use an AED during pregnancy may be at increased risk of being small for their gestational age or for having other birth defects.
- Women with epilepsy should consider taking only one AED during their pregnancy to reduce the risk of birth defects. Taking more than one AED may increase birth defect risk. Carbamazepine is generally considered to be the safest AED for use during pregnancy.
- Of all AEDs, valproate carries the highest risk for birth defects and should be avoided, if possible, during the first trimester. Valproate use has been associated with neural tube defects, facial clefts (cleft lip or palate), and hypospadias (abnormal position of urinary opening on the penis). Valproate may cause poor cognitive outcomes in children exposed to it in the womb. In studies, children born to mothers who took valproate during pregnancy had lower scores on IQ and other cognitive tests than children whose mothers took other types of AEDs. Some research suggests valproate may increase the risk for autism and autism spectrum disorders. Women who take valproate during childbearing years should be sure to use effective birth control.
- Phenytoin and phenobarbital may also cause cognitive impairment.
- Topiramate (Topamax, generic) may increase the risk for cleft lip or palate birth defects when taken during the first trimester of pregnancy.
- Pregnancy can affect how an AED is metabolized in your body. AED levels tend to drop during pregnancy. Your provider should monitor your blood levels throughout your pregnancy to see if your dosage needs to be adjusted. This is especially important if you take lamotrigine, carbamazepine, or phenytoin.
A mother should watch for signs of lethargy or extreme sleepiness in her infant, which could be caused by her medication. Talk with your provider about any concerns you have about breastfeeding and AEDs.
Medications
Anti-epileptic drugs (AEDs) include many types of medications but all act as anticonvulsants.
Seizures can often be controlled using a single-drug regimen. A drug is usually started at a low dose and then slowly increased to a higher dose until the seizures are controlled or side effects occur. If a single drug fails to control seizures, other drugs are added on. The specific drugs and whether more than one should be used are determined by various factors, including a person's age and health condition, and the side effect profile of the drug.
During the first few months of therapy, your health care provider will probably order blood tests to check your liver and kidney function and to monitor drug levels and any side effects. You should let your provider know how you are feeling and if you experience any seizures. Be sure to inform your provider of any medications, herbal remedies, or dietary supplements you take. AEDs can interact with many other drugs.
All antiepileptic drugs can increase the risks of suicidal thoughts and behavior (suicidality). Research has shown that the highest risk of suicide can occur as soon as 1 week after beginning drug treatment and can continue for at least 24 weeks. People who take these drugs should be monitored for signs of depression, changes in behavior, or suicidality.
There are dozens of anti-epileptic drugs. The following are some of the most commonly prescribed.
Valproate
Valproate sodium (Depacon, generic), valproic acid (Depakene, generic), and divalproex sodium (Depakote, generic) are anticonvulsants that are chemically very similar to each other. (In this report, they are collectively referred to as valproate.) Valproate products are the most widely prescribed anti-epileptic drugs worldwide. They are the first choice for people with generalized seizures and are used to prevent nearly all other major seizures as well.
These drugs have a number of side effects that vary depending on dosage and duration. Most side effects occur early in therapy and then subside. The most common side effects are upset stomach and weight gain. Less common side effects include dizziness, hair thinning and loss, and difficulty concentrating.
Serious side effects include:
- A higher risk for serious birth defects than other AEDs especially if taken during the first trimester of pregnancy. In particular, these drugs are associated with facial cleft deformities (cleft lip or palate) and cognitive impairment. [See "Treatment During Pregnancy" in Treatment section.]
- Liver damage or failure is a rare but extremely dangerous side effect that usually affects children who have birth defects and are taking more than one antiseizure drug.
- Pancreatitis (inflammation of the pancreas) and kidney problems are also rare but serious side effects.
Carbamazepine
Carbamazepine (Tegretol, Equetro, Carbatrol, and generic) is used for many types of epilepsy including partial seizures, generalized tonic-clonic (grand mal) seizures, and mixed seizures. A chewable form is available for children.
Common side effects of carbamazepine include dizziness, drowsiness, problems with walking and coordination, nausea, and vomiting.
Carbamazepine can make hormonal forms of birth control less effective. It can also interact with many types of prescription medication.
More serious side effects may include:
- Rare but life-threatening skin reactions, including toxic epidermal necrolysis and Stevens-Johnson syndrome. These skin reactions cause rash, mouth sores, peeling and blistering skin, and other severe symptoms. People of Asian ancestry have a 10 times greater risk for skin reactions than other ethnicities.
- Bone marrow blood disorders such as aplastic anemia and agranulocytosis.
- Be sure to inform your provider if you have sore throat, fever, easy bruising, unusual bleeding, or severe fatigue.
- Long-term therapy may cause bone density loss (osteoporosis) in women.
- Birth defects can occur if taken during pregnancy. This drug may also be passed through breast milk.
Grapefruit, Seville oranges, and tangelos can increase carbamazepine's blood levels and risk of adverse effects.
Phenytoin
Phenytoin (Dilantin, generic) is often prescribed as a first-line drug to treat generalized tonic-clonic (grand mal) seizures and complex partial seizures. This drug may be used alone or in combination with other AEDs.
The most common side effects of phenytoin include problems with walking and coordination, slurred speech, confusion, dizziness, trouble sleeping, and tremor.
More serious side effects may include:
- Softening of the bones (osteomalacia), which can lead to fractures;
- Severe and rare life-threatening skin reactions (Stevens-Johnson syndrome, toxic epidermal necrosis)
- Birth defects if taken during pregnancy
- Drug interactions with other prescription medications
Barbiturates (Phenobarbital and Primidone)
Phenobarbital (Luminal, generic), also called phenobaritone, is a barbiturate anticonvulsant. Primidone (Mysoline, generic) is converted in the body to phenobarbital, and has the same benefits and adverse effects.
Barbiturates may be used to prevent grand mal (tonic-clonic) seizures or partial seizures. They are no longer typically used as first-line drugs, although they may be the initial drug prescribed for newborns and young children.
Many people experience difficulty with side effects. The most common and troublesome side effects or barbiturates are:
- Drowsiness
- Memory problems
- Problems with tasks requiring sustained performance
- Problems with motor skills
- Hyperactivity, particularly in children and the elderly
- Depression
When taken during pregnancy, phenobarbital, like phenytoin and valproate, may lead to impaired cognitive function in the child. There is some evidence that phenobarbitol may cause heart problems in the fetus.
Ethosuximide and Similar Drugs
Ethosuximide (Zarontin, generic) is used for petit mal (absence) seizures in children and adults who have experienced no other type of seizures. Methsuximide (Celontin), a drug similar to ethosuximide, may be suitable as an add-on treatment for intractable epilepsy in children.
This drug can cause stomach problems, dizziness, loss of coordination, and lethargy. In rare cases, it may cause severe and even fatal blood abnormalities.
Clonazepam
Clonazepam (Klonopin, generic) is recommended for myoclonic and atonic seizures that cannot be controlled by other drugs and for Lennox-Gastaut epilepsy syndrome. Although clonazepam can prevent generalized or partial seizures, people generally develop tolerance to the drug, which causes seizures to recur.
People who have had liver disease or acute angle glaucoma should not take clonazepam, and people with lung problems should use the drug with caution. Clonazepam can be addictive, and abrupt withdrawal may trigger status epilepticus. Side effects include drowsiness, imbalance and staggering, irritability, aggression, hyperactivity in children, weight gain, eye muscle problems, slurred speech, tremors, skin problems, and stomach problems.
Lamotrigine
Lamotrigine (Lamictal, generic) is approved as add-on (adjunctive) therapy for partial seizures, and generalized seizures associated with Lennox-Gastaut syndrome, in children aged 2 years and older and in adults.
Lamotrigine is also approved as add-on therapy for treatment of primary generalized tonic-clonic (PGTC) seizures, also known as "grand mal" seizures, in children aged 2 years and older and adults. Lamotrigine can be used as a single drug treatment (monotherapy) for adults with partial seizures. Birth control pills lower blood levels of lamotrigine.
Common side effects include dizziness, headache, blurred or double vision, lack of coordination, sleepiness, nausea, vomiting, insomnia, and rash. Although most cases of rash are mild, in rare cases the rash can become very severe. The risk of rash increases if the drug is started at too high a dose or if used in combination with valproate. (Serious rash is more common in young children who take the drug than it is in adults.) Rash is most likely to develop within the first 8 weeks of treatment. Be sure to immediately notify your provider if you develop a rash, even if it is mild.
Lamotrigine may cause aseptic meningitis. Symptoms of meningitis may include headache, fever, stiff neck, nausea, vomiting, rash, and sensitivity to light. Immediately contact your provider if you experience any of these symptoms.
Gabapentin
Gabapentin (Neurontin, generic) is an add-on drug for controlling complex partial seizures and generalized partial seizures in both adults and children.
Side effects include sleepiness, headache, fatigue, and dizziness. Some weight gain may occur. Children may experience hyperactivity or aggressive behavior.
Pregabalin
Pregabalin (Lyrica) is similar to gabapentin. It is approved as add-on therapy to treat partial-onset seizures in adults with epilepsy.
Side effects include dizziness, sleepiness, dry mouth, swelling in hands and feet, blurred vision, weight gain, and trouble concentrating may occur.
Topiramate
Topiramate (Topamax, generic) is similar to phenytoin and carbamazepine and is used to treat a wide variety of seizures in adults and children. It is approved as add-on therapy for people with generalized tonic-clonic seizures, partial-onset seizures, or seizures associated with Lennox-Gastaut syndrome. It is also approved as single drug therapy.
Most side effects are mild to moderate and can be reduced or prevented by beginning at low doses and increasing dosage gradually. Common side effects may include numbness and tingling, fatigue, abnormalities of taste, difficulty concentrating, and weight loss. Serious side effects may include acute glaucoma and other eye problems. Tell your provider right away if you have blurred vision or eye pain. If used during pregnancy, topiramate may increase the risk for cleft lip or palate birth defects.
Oxcarbazepine
Oxcarbazepine (Trileptal, generic) is similar to phenytoin and carbamazepine but generally has fewer side effects. It is approved as single or add-on therapy for partial seizures in adults and for children ages 4 years and older.
Serious side effects, while rare, include Stevens-Johnson syndrome and toxic epidermal necrolysis. These skin reactions cause a severe rash that can be life threatening. Rash and fever may also be a sign of multi-organ hypersensitivity, another serious side effect associated with this drug. Oxcarbazepine can reduce sodium levels (hyponatremia). Your provider may want to monitor the sodium (salt) level in your blood.
This drug can reduce the effectiveness of birth control pills. Women who take oxcarbazepine may need to use a different type of contraceptive.
Zonisamide
Zonisamide (Zonegran, generic) is approved as add-on therapy for adults with partial seizures.
Zonisamide increases the risk for kidney stones. It may reduce sweating and cause a sudden rise in body temperature, especially in hot weather. Other side effects tend to decrease over time and may include dizziness, forgetfulness, headache, weight loss, and nausea.
Levetiracetam
Levetiracetam (Keppra, generic) is approved both in oral and intravenous forms as add-on therapy for treating many types of seizures in both children and adults.
Side effects tend to occur mostly in the first month. They include sleepiness, dizziness, and fatigue. More serious side effects may include muscle weakness and coordination difficulties, behavioral changes, and increased risk of infections.
Tiagabine
Tiagabine may cause significant side effects including dizziness, fatigue, agitation, and tremor.
Ezogabine
Ezogabine (Potiga), a potassium channel opener, is approved for treatment of partial seizures in adults. Ezogabine is used as an add-on (adjunctive) medication. Its most serious side effect is urinary retention. People who take this drug should be monitored for symptoms such as difficulty initiating urination, weak urine stream, or painful urination.
Other side effects may include coordination problems, memory problems, fatigue, dizziness, and double vision. In 2013, the FDA warned that this drug may cause retina abnormalities, vision loss, and skin discoloration.
Perampanel
Perampanel (Fycompa) is approved as add-on treatment for partial onset seizures in people age 12 years and older. Perampanel is the first in a new class of AEDs for uncontrolled partial epilepsy. It targets the AMPA glutamate receptor, which is involved in seizure activity.
Perampanel is taken as a once-daily tablet. Common side effects may include dizziness, drowsiness, and fatigue. Perampanel also has a boxed warning to alert about potential risks of serious mood changes and mental disturbances including irritability, aggression, anxiety, and violent thoughts or behaviors.
Less Commonly Used AEDs
Felbamate (Felbatol): is an effective antiseizure drug. However, due to reports of deaths from liver failure and from a serious blood condition called aplastic anemia, felbamate is recommended only under certain circumstances. They include severe epilepsy, such as Lennox-Gastaut syndrome, or as monotherapy for partial seizures in adults when other drugs fail. Vigabatrin (Sabril): has serious side effects, such as vision disturbances, and is generally prescribed only in specific cases. It is sometimes given in low doses for children with Lennox-Gastaut syndrome. Vigabatrin is also prescribed as a low-dose oral solution to treat infantile spasms in children ages 1 month to 2 years. Clobazam (Onfi): is a benzodiazepine drug prescribed as add-on treatment for children with Lennox-Gastaut syndrome. It can cause rare but serious skin reactions such as Stevens-Johnson syndrome and toxic epidermal necrolysis. The risk for these reactions is highest during the first 8 weeks of treatment. While these types of serious skin reactions can occur with other AEDs, they are not usually associated with benzodiazepine drugs.
Surgery and Devices
Surgery or surgically implanted neurostimulation devices may be options for people with difficult-to-treat epilepsy that cannot be controlled with medications.
Surgery
Surgery for epilepsy is brain surgery. There are three main types of surgery:
- Resection surgery (lobectomy/lesionectomy)
- Corpus callostomy
- Hemispherectomy
The goal of surgery is to eliminate or at least reduce seizure activity while not causing any functional deficits, such as deterioration of speech or cognitive abilities. Even if surgery is successful, people may still need to take medications for several years following surgery, to help maintain seizure control.
A surgical team will conduct a thorough evaluation prior to any surgery to make sure a person is a good candidate. Various advanced imaging brain scan and mapping techniques are used to provide information on the exact area or areas in the brain that are triggering seizure activity.
It is also important to identify a person's suitability for surgery based on psychological and other medical factors. People with significant psychiatric disorders, or other significant health problems, may not be suitable candidates.
The major areas of the brain have one or more specific functions.
Resection Surgery: Cortical resection surgery involves removing a small part of the brain. The two types of resection surgery are lobectomy and lesionectomy.Lobectomy involves removing an entire lobe of the brain. The most common and successful surgical procedure for epilepsy is anterior temporal lobectomy, which is performed when seizures originate in the temporal lobe. (Surgery is not as successful in epilepsies that occur in the frontal lobe.) It involves removing the front portion of the temporal lobe and small portions from the hippocampus and often the amygdala.
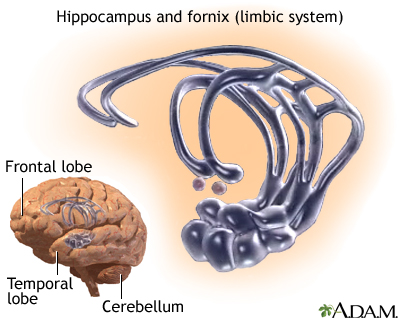
The hippocampus is contained in the temporal lobe and is a part of the brain that is involved in memory processing. It is part of the limbic system, which controls emotions. Temporal lobectomy successfully reduces or eliminates seizures in most people, but can cause problems with memory and learning.
Lesionectomies are performed to remove damaged or abnormal tissue that is causing seizure activity. These lesions may be congenital (present at birth) such as cortical dysplasia. Lesions may also be due to other acquired conditions such as strokes or head trauma.
Corpus callostomy: Corpus callostomy disconnects the nerve connections between the right and left sides (hemispheres of the brain). The surgeon cuts into the band of tissue that connects these hemispheres to prevent seizures from becoming generalized and spreading from one side of the brain to the other. However, this procedure does not stop seizures from continuing to occur in one side of the brain. Hemispherectomy: Children who have extremely severe seizures that originate on only one side of the brain may be candidates for hemispherectomy. This is a radical surgical procedure that involves removing a large portion of one side of the brain.Neurostimulation Devices
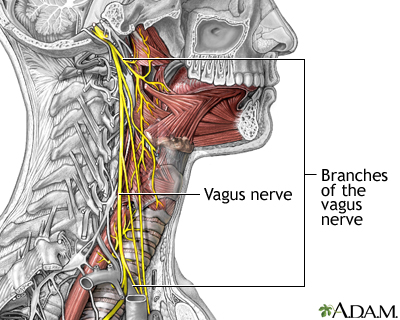
Electrical stimulation of areas in the brain that affect epilepsy can help many people with refractory epilepsy. Neurostimulators are sometimes called "pacemakers for the brain." In 1997, the FDA first approved vagus nerve stimulation (VNS) for treating people with partial epilepsy whose seizures were not helped by medication. In 2013, the FDA approved a second neurostimulation device, the RNS stimulator. Researchers are continuing to study other types of brain stimulation devices as treatments for epilepsy.
Vagus nerve stimulation (VNS): Electrical stimulation of the vagus nerve is an accepted therapy for severe epilepsy that does not respond to medication. The two vagus nerves are the longest nerves in the body. They run from the brain stem and down through each side of the neck, and then pass through the esophagus to the gastrointestinal tract. They affect swallowing, speech, and many other functions. They also appear to connect to parts of the brain that are involved with seizures.The VNS procedure is as follows:
- A battery-powered device similar to a pacemaker is implanted under the skin in the upper left of the chest.
- A lead is then attached to the left vagus nerve in the lower part of the neck.
- The neurologist programs the device to deliver mild electrical stimulation to the vagus nerve. (People may also pass a magnet over the device to give it an extra dose if they sense a seizure coming on.)
- The batteries wear out after 5 to 10 years and need to be removed and replaced by a simple surgical procedure.
VNS is FDA-approved for people with partial epilepsy and those whose seizures are not helped by medication. According to the most recent guidelines from the American Academy of Neurology, there is weak evidence that VNS may help as added therapy for children with Lennox-Gastaut syndrome, and children and adults with generalized or partial epilepsy. There is also weak evidence that VNS may possibly help improve depression and mood problems in people with epilepsy.
VNS can help reduce seizure frequency and how long seizures last. For side effects, VNS can cause shortness of breath, hoarseness, sore throat, coughing, ear and throat pain, or nausea and vomiting. These side effects can be reduced or eliminated by reducing the intensity of stimulation.
Some studies suggest that the treatment causes adverse changes in breathing during sleep and may cause lung function deterioration in people with existing lung disease. People who have obstructive sleep apnea should be cautious about this procedure. Turning off the VNS (for example before an MRI or surgery) may increase the risk for status epilepticus. (However, VNS may also be helpful for treating status epilepticus in some people.)
Responsive neurostimulation (RNS Stimulator): In 2013, the FDA approved a new type of neurostimulator device called the RNS stimulator. What makes RNS different from VNS is that it is a responsive stimulation system. RNS detects abnormal electrical activity in the brain and responds by sending electrical stimulation. In other words, the device can help stop seizures before they occur.The RNS system is approved for adults with partial onset seizures that could not be controlled with two or more anti-epileptic drugs. The RNS Stimulator will not completely eliminate seizures, but can help reduce seizure frequency. In clinical trials, the most common side effect was infection at the implant site. People who have an RNS stimulator implanted cannot undergo MRI procedures.
Lifestyle Changes
Epilepsy is a chronic and usually lifelong condition. Seizures cannot be prevented by lifestyle changes alone, but people can make behavioral changes that improve their lives and give them a sense of control.
Avoiding Epileptic Triggers
In most cases, there is no known cause for epileptic seizures, but specific events or conditions may trigger them and should be avoided.
Poor sleep: Inadequate or fragmented sleep can set off seizures in many people. Using sleep hygiene or other methods to improve sleep may be helpful. Food allergies: Specific foods are not generally associated with seizures but may have an effect in certain people. If you suspect that a food is a seizure trigger, try keeping a diary of what you eat and when your seizures occurred. Check with your health care provider if certain foods may interact with any medications you are taking. Alcohol and smoking: Alcohol and smoking should be avoided. Light alcohol consumption does not usually increase seizure activity in people who are not alcohol dependent or sensitive to alcohol. Heavy alcohol use can trigger seizures, as can cigarette smoking. Flashing lights: Avoid exposure to flashing or strobe lights. Video games have been known to trigger seizures in people with existing epilepsy, but apparently only if they are already sensitive to flashing lights. Seizures have been reported among people who watch cartoons with rapidly fluctuating colors and quick flashes.Relaxation Techniques
Relaxation methods include deep breathing, biofeedback, and meditation techniques. No strong evidence supports their value on reducing seizures (although some people benefit), but they may be helpful in reducing anxiety.
Exercise
Exercise is important for many aspects of epilepsy, although it can be problematic. Weight-bearing exercise helps maintain bone density, which can be reduced by some medications. Exercise can help to prevent weight gain, which is a problem with some drugs. Exercise is also helpful for preventing depression and maintaining good emotional and psychological health.
People with epilepsy do need to take certain precautions to exercise safely. These include making sure not to get too hot or tired, which may trigger seizures. They should refrain from sports that might cause injuries to the head.
Swimming is great exercise, but drowning is a serious risk for people with epilepsy. Make sure that you have a companion with you when you go swimming who can recognize the signs of a seizure and knows what to do if you have one. It is also safest to swim at a pool that has a life guard on duty.
The Ketogenic Diet
The ketogenic diet is very high in fat (90%), very low in carbohydrates, and low in protein. It appears to be helpful for many children with severe epilepsy. Some children who try the ketogenic diet are able to stop or at least reduce their medications.
It is not clear how the ketogenic diet works. The standard theory is that burning fat instead of carbohydrates causes an increase in ketones (chemical substances in the body that result from the breakdown of fat in the body). When excessive levels of ketones are produced, a metabolic state called ketosis happens. Ketosis appears to alter certain amino acids in the brain and to increase levels of the neurotransmitter gamma aminobutyric acid (GABA), which helps prevent nerve cells from over-firing.
This diet must be professionally monitored. Parents can endanger their children if they try the program on their own without consulting a doctor or trained dietician.
The child fasts for the first 1 to 2 days, and then the diet is gradually introduced. The regimen uses small amounts of carbohydrates and large amounts of fats (up to 90%), with very few proteins and no sugar. Children generally consume 75% of their usual daily calorie requirements.
A typical dinner may include a chicken cutlet or piece of fish, broccoli with cheese, lettuce with mayonnaise, and a whipped cream sundae. Vegetables may include celery, cucumbers, or asparagus, cauliflower, and spinach. Breakfast might consist of an omelet, bacon, and cocoa with cream. (Artificial sweeteners are used for any desserts.)
The diet is very complex and difficult, as a slight deviation from the diet can provoke a seizure. Children cannot take medications that contain sugar (which is common in many drugs produced for children). Some sunscreens and lotions contain sorbitol, a carbohydrate that can be absorbed through skin. Many children and parents find the diet too difficult or ineffective and stop it after 6 months.
Researchers are investigating a modified version of the popular Atkins diet, which does not require the caloric, protein, or fluid restrictions of the ketogenic diet. Unlike the traditional Atkins diet, the modified Atkins diet uses less carbohydrates and fatter intake. Another alternative is a low glycemic index diet, which contains even fewer carbohydrates than the Atkins diet. Still, parents should not put their children on these diets without support from a health care provider.
Side Effects and Complications: To prevent serious side effects, children need regular monitoring by a health care provider, especially when the ketogenic diet is first initiated.Side effects or complications that may occur at the start of the diet include:
- Acidosis, a build-up of acid in the blood and body
- Low blood sugar (hypoglycemia)
- Stomach upset
- Dehydration
- Lethargy
Side effects that may occur later on include:
- Unhealthy cholesterol and lipid levels
- Vitamin and mineral deficiencies (supplements may be needed)
- Kidney stones, which may be a complication of acidosis.
- Slowing of growth (tends to occur more in younger children than older children)
- Decreased bone density
Because most children remain on the diet for only 2 years, the risks for potential long-term damage appear minimal.
Emotional and Psychological Support
Many people with epilepsy and their family members can benefit from support associations. These services are usually free and available in most cities.
People with epilepsy often contend with depression and other mental health issues. Psychological therapy may be helpful. Cognitive behavioral therapy offers a structured counseling program that helps people change behaviors associated with seizure triggers, such as anxiety and insomnia.
Tips for helping children: Some of the following tips may help children with epilepsy:- Children should be treated as normally as possible by parents and siblings.
- Children should be assured that they will not die from epilepsy.
- Most children will not have seizures triggered by sports or by any other ordinary activities that are enjoyable and healthy.
- As soon as they are old enough, children should be active participants in maintaining their drug regimens.
Medical Marijuana
Several American states have legalized the sale of medical marijuana. Some parents of children with epilepsy have turned to medical marijuana as a possible treatment when their children's seizures have not been helped by medication. According to organizations such as the American Epilepsy Society and American Academy of Neurology, there is currently not enough evidence to know whether the cannabinoids in marijuana are safe and effective for reducing seizure activity.
Resources
- www.epilepsyfoundation.org -- Epilepsy Foundation
- www.aesnet.org -- American Epilepsy Society
- www.aan.com -- American Academy of Neurology
- www.ninds.nih.gov -- National Institute of Neurological Disorders and Stroke
References
Bell GS, Gaitatzis A, Bell CL, Johnson AL, Sander JW. Drowning in people with epilepsy: how great is the risk? Neurology. 2008;71(8):578-582.
Bell GS, Gaitatzis A, Bell CL, Johnson AL, Sander JW. Suicide in people with epilepsy: how great is the risk? Epilepsia . 2009;50(8):1933-1942.
Christensen J, Grønborg TK, Sørensen MJ, et al. Prenatal valproate exposure and risk of autism spectrum disorders and childhood autism. JAMA . 2013;309(16):1696-1703.
Christensen J, Vestergaard M, Mortensen PB, Sidenius P, Agerbo E. Epilepsy and risk of suicide: a population-based case-control study. Lancet Neurol . 2007;6(8):693-698.
Fiest KM, Dykeman J, Patten SB, et al. Depression in epilepsy: a systematic review and meta-analysis. Neurology . 2013;80(6):590-599.
Fisher RS, Acevedo C, Arzimanoglou A, Bogacz A, Cross JH, Elger CE, et al. ILAE official report: a practical clinical definition of epilepsy. Epilepsia . 2014 Apr;55(4):475-82. doi: 10.1111/epi.12550. Epub 2014 Apr 14. PMID: 24730690 www.ncbi.nlm.nih.gov/pubmed/24730690 .
Freeman JM, Kossoff EH, Hartman AL. The ketogenic diet: one decade later. Pediatrics . 2007 Mar;119(3):535-543.
French JA, Pedley TA. Clinical practice. Initial management of epilepsy. N Engl J Med . 2008 Jul 10;359(2):166-176.
Gloss D, Vickrey B. Cannabinoids for epilepsy. Cochrane Database Syst Rev . 2014 Mar 5;3:CD009270. PMID: 24595491 www.ncbi.nlm.nih.gov/pubmed/24595491 .
Harden CL, Hopp J, Ting TY, et al. Practice parameter update: management issues for women with epilepsy--focus on pregnancy (an evidence-based review): obstetrical complications and change in seizure frequency: report of the Quality Standards Subcommittee and Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and American Epilepsy Society. Neurology . 2009 Jul 14;73(2):126-132.
Harden CL, Meador KJ, Pennell PB, et al. Practice parameter update: management issues for women with epilepsy -- focus on pregnancy (an evidence-based review): teratogenesis and perinatal outcomes: report of the Quality Standards Subcommittee and Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and American Epilepsy Society. Neurology . 2009;73(2):133-141.
Harden CL, Pennell PB, Koppel BS, et al. Practice parameter update: management issues for women with epilepsy--focus on pregnancy (an evidence-based review): vitamin K, folic acid, blood levels, and breastfeeding: report of the Quality Standards Subcommittee and Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and American Epilepsy Society. Neurology. 2009;73(2):142-149.
Hernández-Díaz S, Smith CR, Shen A, et al. Comparative safety of antiepileptic drugs during pregnancy. Neurology . 2012;78(21):1692-1699.
Hirsch LJ, Donner EJ, So EL, et al. Abbreviated report of the NIH/NINDS workshop on sudden unexpected death in epilepsy. Neurology . 2011;76(22):1932-1938.
Koppel BS, Brust JC, Fife T, Bronstein J, Youssof S, Gronseth G, et al. Systematic review: efficacy and safety of medical marijuana in selected neurologic disorders: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2014 Apr 29;82(17):1556-63. PMID: 24778283 www.ncbi.nlm.nih.gov/pubmed/24778283 .
Kossoff EH, Zupec-Kania BA, Rho JM. Ketogenic diets: an update for child neurologists. J Child Neurol. 2009;24(8):979-988.
Krumholz A, Wiebe S, Gronseth G, et al. Practice Parameter: evaluating an apparent unprovoked first seizure in adults (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology . 2007;69(21):1996-2007.
Kwan P, Schachter SC, Brodie MJ. Drug-resistant epilepsy. N Engl J Med . 2011;365(10):919-926.
Meador KJ, Baker GA, Browning N, et al. Cognitive function at 3 years of age after fetal exposure to antiepileptic drugs. N Engl J Med . 2009;360(16):1597-1605.
Mølgaard-Nielsen D, Hviid A. Newer-generation antiepileptic drugs and the risk of major birth defects. JAMA . 201118;305(19):1996-2002.
Morris GL 3rd, Gloss D, Buchhalter J, et al. Evidence-based guideline update: vagus nerve stimulation for the treatment of epilepsy: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology . 2013;81(16):1453-1459.
Shorvon SD, Goodridge DM. Longitudinal cohort studies of the prognosis of epilepsy: contribution of the National General Practice Study of Epilepsy and other studies. Brain. 2013;136(Pt 11):3497-3510.
Review Date: 4/1/2015
Reviewed By: Daniel Kantor, MD, Kantor Neurology, Coconut Creek, FL and Immediate Past President of the Florida Society of Neurology (FSN). Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team. Author: Julia Mongo, MS.