Sinusitis
Nasal congestion; Rhinosinusitis
An in-depth report on the causes, diagnosis, treatment, and prevention of sinusitis.
Highlights
Sinusitis is an infection or inflammation of the sinuses, the air-filled chambers in the skull that are located around the nose. Symptoms of sinusitis include thick nasal discharge, facial pain or pressure, fever, and reduced sense of smell. Depending on how long these symptoms last, sinusitis is classified as acute, chronic, or recurrent.
Viruses are the most common cause of acute sinusitis, but bacteria are responsible for most of the serious and chronic cases.
Non-Drug Treatment of SinusitisHome remedies such as nasal saline (salt) washes are helpful for removing mucus and relieving congestion. People with sinusitis should drink plenty of fluids to avoid dehydration. Water, which helps lubricate the mucous membranes, is the best fluid to drink.
Drug Treatment of SinusitisMedication depends on the type of sinusitis and its cause. Nonprescription pain relievers such as acetaminophen and ibuprofen can help mild-to-moderate pain. Decongestants may help relieve congestion, but they do not cure sinusitis. Antihistamines are not generally recommended because they can dry the mucus and worsen the condition; however, they may be used when sinusitis is associated with allergies. Cough or cold medication is not recommended for children younger than age 4.
Because many cases of acute sinusitis resolve within 2 weeks with nonprescription treatments and home remedies, health care providers generally wait at least 7 days before prescribing an antibiotic.
For chronic sinusitis, nasal corticosteroids and antibiotics are the main treatments. Other drugs may also be prescribed. If drugs are ineffective, some people with chronic sinusitis may need surgery.
Introduction
Sinusitis (also called rhinosinusitis) is inflammation of the mucous lining of the nasal passages and sinus cavities. The sinuses are air-filled chambers in the skull (behind the forehead, nasal bones, cheeks, and eyes) that are lined with mucous membranes.
Four pairs of sinuses, known as the paranasal air sinuses , connect to the nasal passages (the two airways running through the nose):
- Frontal sinuses (behind the forehead)
- Maxillary sinuses (behind the cheekbones)
- Ethmoid sinuses (behind the nose)
- Sphenoid sinuses (behind the eyes)
Sinusitis occurs if obstruction or congestion causes the paranasal sinus openings to become blocked. When the sinus openings become blocked or too much mucus builds up in the chambers, bacteria and other germs can grow more easily, leading to infection and inflammation.
Sinusitis is classified as acute, chronic, or recurrent. The classification is based on how long symptoms last:
- Acute: Less than 4 weeks. Can be caused by virus or bacteria.
- Chronic: 12 weeks or longer. Is due to prolonged inflammation.
- Recurrent: 4 or more acute episodes in 1 year or symptoms lasting between 4 and 8 weeks.
Sinusitis is always accompanied (and usually preceded) by rhinitis, which is inflammation of the mucous membrane of the nasal cavities. The two conditions share common symptoms such as nasal obstruction and discharge.
Causes
Acute sinusitis can be caused by viral, bacterial, or fungal infections. Allergens and environmental irritants are other possible causes. In most cases, acute sinusitis is caused by an upper respiratory tract viral infection, such as the common cold, and usually resolves on its own.
Chronic sinusitis refers to long-term swelling and inflammation of the sinuses. Chronic sinusitis can result from recurring episodes of acute sinusitis, or it can be caused by other health conditions, like:
- Asthma and allergic rhinitis
- Immune disorders
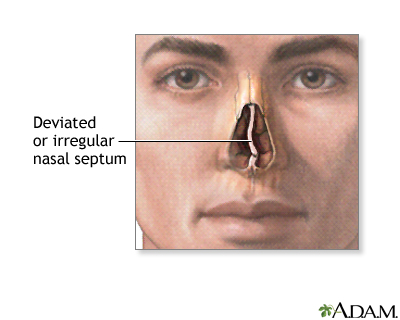
- Structural abnormalities in the nose, like a deviated septum or nasal polyps
Viral, Bacterial, and Fungal Infections
Viruses: Viruses cause 90 to 98% of acute sinusitis cases. Acute sinusitis typically starts with the common cold virus. A cold can set the stage for sinusitis by causing inflammation and congestion in the nasal passages, leading to obstruction in the sinuses. Bacteria: A small percentage of acute sinusitis, and possibly chronic sinusitis cases, are caused by bacteria. Bacteria are normally present in the nasal passages and throat and are usually harmless. However, when a cold or other viral upper respiratory infection blocks the nasal passage and prevents the sinuses from draining, bacteria can multiply within the mucous lining of the sinuses, causing sinusitis.Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis (a common cause of childhood illnesses) are the bacteria most often linked to acute sinusitis. These bacteria plus other strains, such as Staphylococcus aureus , are also associated with chronic sinusitis. (The role of bacteria in chronic sinusitis is still being debated.) Bacterial sinusitis usually causes more severe symptoms and lasts longer than viral sinusitis.
Fungi: An allergic reaction to fungi is a cause of some chronic rhinosinusitis cases. Aspergillus is the most common fungus associated with sinusitis. Fungal infections tend to occur in people with sinusitis who also have diabetes, leukemia, AIDS, or other conditions that impair the immune system. Fungal infections can also occur in people with healthy immune systems, but they are far less common.Allergies, Asthma, and Immune Response
Allergies, asthma, and sinusitis often overlap. Seasonal allergic rhinitis and other allergies that cause mucus blockage may predispose people to develop sinusitis. Many of the immune factors observed in people with chronic sinusitis resemble those that appear in allergic rhinitis, suggesting that in some people sinusitis is due to an allergic response.
Asthma is also strongly associated with sinusitis and many people have both conditions. Some studies suggest that sinusitis may worsen asthma symptoms.
Chronic sinusitis and recurrent acute sinusitis are also associated with disorders that weaken the immune system or produce airway inflammation or persistent thickened stagnant mucus. These conditions include diabetes, AIDS, cystic fibrosis, Kartagener syndrome, and Wegener granulomatosis.
Structural Abnormalities of the Nasal Passage
Structural abnormalities in the nose can cause a blockage, thereby increasing the risk for chronic sinusitis. These abnormalities include:
- Polyps (small benign growths) in the nasal passage that block mucus drainage and may restrict airflow. Polyps can result from previous sinus infections that caused overgrowth of the nasal membrane.
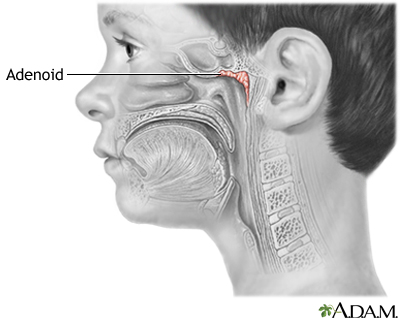
- Enlarged adenoids can lead to sinusitis.
Adenoids are masses of tissue located high on the posterior wall of the pharynx. They are made up of lymphatic tissue, which trap and destroy germs in the air that enter the nasopharynx.
- Cleft palate
- Tumors
- Deviated septum (a common structural abnormality in which the septum, the midline cartilage separating the two sides of the nose, is shifted to one side)
Risk Factors
Sinusitis is a very common disease.
Young Children and Sinusitis
Before the immune system matures, all infants are susceptible to respiratory infections. Babies catch a cold about every 1 to 2 months. Young children are prone to colds and may have 8 to 12 bouts every year. Smaller nasal and sinus passages make children more vulnerable to upper respiratory tract infections than older children and adults. Ear infections such as otitis media are also associated with sinusitis.
The Elderly and Sinusitis
Older people are at heightened risk for sinusitis. Their nasal passages tend to dry out with age. In addition, the cartilage supporting the nasal passages weakens, causing airflow changes. They also have diminished cough and gag reflexes and weakened immune systems and are at greater risk for serious respiratory infections than are young and middle-aged adults.
People with Asthma or Allergies
People with asthma or allergies are at increased risk for inflammation in the sinuses. People with a combination of polyps in the nose, asthma, and sensitivity to aspirin (called Samter's, or ASA, triad) are at very high risk for chronic or recurrent acute sinusitis.
Hospitalization
Some hospitalized people are at higher risk for sinusitis, particularly those with:
- Head injuries
- Conditions requiring insertion of tubes through the nose
- Breathing aided by mechanical ventilators
- Weakened immune system
Other Medical Conditions Affecting the Sinuses
A number of medical conditions put people at risk for chronic sinusitis. They include:
- Diabetes (types 1 and 2)
- Gastroesophageal reflux disease
- Nasal polyps or septal deviation
- AIDS and other disorders of the immune system
- Oral or intravenous steroid treatment
- Hypothyroidism (underactive thyroid gland)
- Cystic fibrosis, a genetic disorder in which the mucus is very thick and builds up
- Kartagener syndrome, a genetic disorder that impairs function of cilia, the hair-like structures that normally move mucus through the respiratory tract
Miscellaneous Risk Factors
Dental Problems: Bacteria associated with infections from dental problems or procedures can trigger cases of maxillary sinusitis. Changes in Atmospheric Pressure: People who experience changes in atmospheric pressure, such as while flying, may face an increased risk of developing sinusitis. Cigarette Smoke and Other Air Pollutants: Air pollution from industrial chemicals, cigarette smoke, or other pollutants can damage the cilia responsible for moving mucus through the sinuses. It is still not clear whether air pollution is an important cause of sinusitis and which specific pollutants are critical factors. Cigarette smoke, for example, poses a small but definite risk for sinusitis in adults. Secondhand smoke does not appear to have any significant effect on adult sinuses, although it may pose a risk for sinusitis in children.
Complications
Bacterial Infections
Bacterial sinusitis is nearly always harmless (although uncomfortable and sometimes even very painful). If an episode becomes severe, antibiotics generally eliminate further problems. In rare cases, however, bacterial sinusitis can cause very serious infections.
Infection of the Frontal Bone: Osteomyelitis is infection of the bones. In rare cases, sinusitis can lead to infection of the forehead and other facial bones. In such cases, the person usually experiences headache, fever, and a soft swelling over the bone known as Pott puffy tumor. Infection of the Eye Socket: Infection of the eye socket (orbital cellulitis), which causes swelling and subsequent drooping of the eyelid, is a rare but serious complication of ethmoid sinusitis. In these cases, the person loses movement in the eye, and pressure on the optic nerve can lead to vision loss, which is sometimes permanent. Fever and severe illness are usually present. Brain Infection: The most dangerous complication of sinusitis, particularly frontal and sphenoid sinusitis, is the spread of infection by anaerobic bacteria to the brain, either through the bones or blood vessels. Abscesses, meningitis, and other life-threatening conditions may result. In such cases, the person may experience mild personality changes, headache, altered consciousness, visual problems, and, finally, seizures, coma, and death.Blood Clots
Blood clots are another danger, although rare, from ethmoid or frontal sinusitis. If a blood clot forms in the sinus area around the front and top of the face, symptoms are similar to infection of the eye socket. In addition, the pupil may be fixed and dilated. Although symptoms usually begin on one side of the head, the process usually spreads to both sides.
Increased Asthma Severity
Many people with moderate-to-severe asthma also have sinusitis and allergic rhinitis. The relationship between sinusitis and asthma is not clear, but sinusitis appears to predispose people to more severe asthma attacks. Evidence suggests that treating one condition can have a beneficial impact on the other.
Effect on Quality of Life
Pain, fatigue, and other symptoms of chronic sinusitis can have significant effects on quality of life. This condition can cause emotional distress, impair normal activity, and reduce attendance at work or school. According to the American Academy of Allergy, Asthma, and Immunology, the average person with sinusitis misses about 4 work days a year, and sinusitis is one of the top 10 medical conditions that most adversely affect employers.
Symptoms
General Symptoms of Acute Sinusitis
Sinus symptoms are very common during a cold or the flu. In most cases, they are due to the effects of the infecting virus and resolve when the infection does. General symptoms of acute sinusitis (both viral and bacterial) include:
- Nasal congestion or discharge
- Headache
- Facial pain, pressure, or feeling of fullness
- Cough or scratchy throat
- Fever
- Diminished or absent sense of smell
- Other symptoms, such as ear pain or pressure, dental pain, bad breath, and fatigue
Acute Bacterial Sinusitis Symptoms
It is important to differentiate between inflamed sinuses associated with cold or flu virus and sinusitis caused by bacteria, but it can be difficult to do so. In general, with viral sinusitis, symptoms usually last 7 to 10 days and then improve. Acute bacterial sinusitis, in contrast to viral sinusitis, usually takes one of the following three paths:
- Persistent symptoms that last more than 10 days and do not improve. Nasal discharge (either clear or colored) and daytime cough are common.
- Severe symptoms, with a high fever (at least 102oF [38.8oC]) and thick, green nasal discharge or facial pain that lasts for at least 3 to 4 days starting from the beginning of the illness. (With viral sinusitis, fever usually disappears within the first day or two and green discharge does not appear until after the fourth day.)
- Worsening symptoms following a typical viral upper respiratory infection. Symptoms appear to improve but are then followed suddenly by another set of worsening symptoms (return of fever, cough, severe headache, or increase in nasal discharge) after 5 to 6 days ("double-sickening").
If symptoms suggest acute bacterial sinusitis, antibiotic treatment is warranted. Bacterial sinusitis is not as common as viral sinusitis, but bacteria are responsible for most serious cases of sinusitis.
Children: In children, the most common signs and symptoms of acute bacterial sinusitis are daytime cough (which may worsen at night), nasal discharge, and fever. Bad breath, fatigue, headache, and decreased appetite are also common symptoms in young children, but they do not necessarily indicate sinusitis.The American Academy of Pediatrics recommends that health care providers diagnose acute bacterial sinusitis when a child with an upper respiratory infection has:
- Symptoms that last more than 10 days
- Severe onset of symptoms (including fever and nasal discharge) lasting at least 3 days in a row
- Symptoms (like nasal discharge, fever, or cough) that get worse after initially improving
Children with worsening or severe symptoms should be treated with antibiotics. For other children, watchful waiting is appropriate to see if the infection clears up on its own.
Chronic Sinusitis Symptoms
With chronic sinusitis:
- Any of the sinusitis symptoms listed previously may be present
- Symptoms are more vague and generalized than with acute sinusitis
- Fever may be absent or low-grade
- Symptoms of sinusitis last 12 weeks or longer
- Symptoms occur throughout the year, even during nonallergy seasons
Symptoms Indicating a Medical Emergency
Rare complications of sinusitis can produce additional symptoms, which may be severe or even life-threatening. Symptoms indicating a medical emergency include:
- Increasing severity of symptoms
- Eyes that are red, bulging, or painful (if the sinus infection occurs around the eyes)
- Swelling and drooping eyelid
- Loss of eye movement (possible infection in the eye socket)
- Vision changes
- Fixed or dilated pupil
- Symptoms spreading to both sides of face (may indicate blood clot)
- Development of severe headache, altered vision
- Mild personality or mental changes (may indicate spread of infection to brain)
- Soft swelling over the bone (may indicate bone infection)
Other Causes of Sinusitis Symptoms
Allergies: Symptoms of both sinusitis and allergic rhinitis include nasal obstruction and congestion. The conditions often occur together. People with allergies and no sinus infection may have:- Thin, clear, and runny nasal discharge
- Itchy nose, eyes, or throat (these symptoms do not occur with bacterial sinusitis)
- Recurrent sneezing
- Symptoms of allergies that appear only during exposure to allergens
- Dental problems
- A foreign object in the nasal passage
- Temporal arteritis (headache caused by inflamed arteries in the head)
- Persistent upper respiratory tract infections
- Temporomandibular disorders (problems in the joints and muscles of the jaw hinges)
- Vasomotor rhinitis, a condition in which the nasal passages become congested in response to irritants or stress. It often occurs in pregnant women.
Diagnosis
See your health care provider if you have sinusitis symptoms that do not clear up within a few days, are severe, or are accompanied by high fever or sudden generalized illness.
The first goal in diagnosing sinusitis is to rule out other possible causes of symptoms, and then determine:
- The site where the infection has occurred
- Whether the condition is acute or chronic
- Whether the condition is caused by virus or bacteria
Diagnostic Approach to Acute Sinusitis
Medical History: You should describe to your provider all of your symptoms, such as nasal discharge and specific pain in the face and head, including eye and tooth pain.The provider will evaluate your symptoms and take a thorough medical history, including:
- Any history of allergies, asthma, or headaches
- Recent upper respiratory infections (colds, flu, and infection) and how long they lasted
- History of sinusitis episodes that did not respond to antibiotic treatment.
- Exposure to cigarette smoke or other environmental pollutants
- Recent air travel
- Recent dental procedures
- Medications (particularly decongestants)
- Any known structural abnormalities in the nose and face
- Injury to the head or face
- History of medical conditions that can produce tender areas in the face or sinus regions, and nonspecific symptoms of ill health
- Any family or personal history of immune disorders, cystic fibrosis, or Kartagener syndrome
The provider will ask how long your symptoms have lasted:
- If you have been sick less than 10 days and your symptoms are not getting worse, you likely have acute viral sinusitis .
- If you have been sick at least 10 days and have not improved or your symptoms worsened after beginning to feel better ("double sickening"), you likely have acute bacterial sinusitis . Symptoms such as high fever and thick, colored nasal discharge may indicate a bacterial infection.
- It is important to diagnose if you have sinusitis caused by virus or bacteria because the treatment approaches are different.
Physical Examination
The provider will press the forehead and cheekbones to check for tenderness and other signs of sinusitis, including yellow to yellow-green nasal discharge. The doctor will also check the inside of the nasal passages using a device with a bright light to look for, nasal obstruction and any structural abnormalities.
Nasal Endoscopy
Nasal endoscopy (NE) involves the insertion of a flexible tube with a fiberoptic light on the end into the nasal passage. NE allows detection of even very small abnormalities in the nasal passages. It can evaluate structural problems of the nasal septum, as well as the presence of soft tissue growths such as polyps. NE may also identify small amounts of pus draining from the opening of a sinus. Bacterial cultures can be taken from samples removed using endoscopy. NE is also used for treating sinusitis.
Imaging Tests
Imaging tests are not usually needed to diagnose acute sinusitis.
Computed Tomography (CT): CT scanning is the best method for viewing the paranasal sinuses. However, CT scans are not recommended for most cases of uncomplicated acute bacterial sinusitis. They are only recommended for acute sinusitis if there is a severe infection, complications, or a high risk for complications, especially those that may affect the eyes or central nervous system.CT scans can be useful for diagnosing chronic or recurrent acute sinusitis and for planning operations. They show inflammation and swelling and the extent of the infection, including in deeply hidden air chambers that x-rays and nasal endoscopy may miss. They may also detect fungal infections.
X-Rays: X-rays used to be commonly used, but they are not as accurate as endoscopy and CT scans for identifying abnormalities in the sinuses, particularly the ethmoid sinuses.Sinus Puncture and Bacterial Culture
Sinus puncture with bacterial culture, while very sensitive for diagnosing a bacterial sinus infection, is not commonly done. It is invasive and can be painful, and is performed only when people are at risk of having unusual infections or serious complications, or if antibiotics have not worked.
Sinus puncture involves using a needle to withdraw a small amount of fluid from the sinuses. It requires a local anesthetic and is performed by a specialist. More routinely, the gold standard has become endoscopic-guided cultures which can be done at the time of office endoscopy and is much less invasive with similar accuracy. In either case, the fluid is then cultured to determine what type of bacteria is causing sinusitis.
Prevention
The best way to prevent sinusitis is to avoid colds and influenza. If you are unable to avoid these viruses, the next best way to prevent sinusitis is to effectively treat colds and influenza.
Good Hygiene and Preventing Transmission
Cold and flu viruses spread when an infected person coughs or sneezes. These viruses can also be transmitted by shaking hands. Everyone should always wash their hands before eating and after going outside. Ordinary soap is sufficient. Waterless hand cleansers that contain an alcohol-based gel are also effective. Antibacterial soaps add little protection, particularly against viruses. Wiping surfaces with a solution that contains 1 part bleach to 10 parts water is very effective in killing viruses.
Vaccines
Influenza Vaccine: Most people should receive an annual influenza vaccination in October or November. Because influenza viruses change from year to year, influenza vaccines are redesigned annually to match the anticipated viral strains.Flu vaccines are now recommended for virtually everyone over 6 months of age, except for those allergic to eggs or other vaccine compounds.
Flu vaccines
An in-depth report on the diagnosis, treatment, and prevention of colds and flu.

|
|
|
| Read Article Now | Book Mark Article |
Vaccines
OverviewBacteria, viruses, parasites, and other germs (microbes) cause many human diseases. Vaccines can help protect against some of these microbes...

|
|
|
| Read Article Now | Book Mark Article |
Treatment
General Treatment Approaches
General treatment goals for sinusitis aim to:
- Reduce swelling
- Stop infection
- Drain the sinuses
- Ensure that the sinuses remain open
Most people with sinusitis do not require aggressive treatment. Home remedies such as nasal salt water (saline) washes and drinking plenty of fluids can be very helpful. Medications may be given if necessary. Ask your health care provider before taking an antihistamine (like Benadryl, Claritin, or Zyrtec) which may or may not be helpful for sinusitis. Specific treatment approaches depend on whether sinusitis is acute or chronic, and whether it is caused by a virus or bacteria.
Treatment of Acute Viral Sinusitis: Most cases of sinusitis are caused by viruses, which do not respond to antibiotics. Acute viral sinusitis generally clears up on its own within 7 to 10 days. Symptoms of acute viral sinusitis can be treated with nasal saline washes, pain relievers like ibuprofen (Advil, generic) and acetaminophen (Tylenol, generic), and nasal spray corticosteroids. Treatment of Acute Bacterial Sinusitis: Bacterial sinusitis accounts for only 2 to 10% of acute sinusitis cases. Antibiotics can treat bacterial infection, but not all cases of acute bacterial sinusitis require antibiotic treatment. Guidelines for treatment of acute bacterial sinusitis recommend:- Watchful waiting for up to 7 days to see if the sinusitis clears up on its own. Your provider may give you a prescription for an antibiotic to take if you do not get better after 7 days or if your sinusitis worsens during this time.
- If an antibiotic is needed, amoxicillin with or without clavulanate is recommended. You will take the antibiotic for 5 to 10 days.
- For children who have symptoms for more than 10 days, doctors may wait and watch for an additional 3 days before prescribing antibiotics to see if the infection clears up on its own. Children who have severe or worsening symptoms should receive immediate treatment with antibiotics.
- For symptom relief, use saline nasal rinses, pain relievers, and decongestants. Do not use nasal decongestants for more than 3 days in a row. Nasal steroid sprays are another option, but have limited benefit.
- Corticosteroid nasal sprays and saline nasal irrigation are standard treatments.
- A thorough diagnostic workup should be performed to rule out any underlying conditions, including allergies, asthma, immune system problems, gastroesophageal reflux disorder, and structural problems in the nasal passages. If a primary trigger for chronic sinusitis can be identified, it should be treated or controlled.
- If there is no improvement, surgery may be considered. For some people with chronic sinusitis the condition is not curable, and the goal of treatment is to improve the quality of life.
- The role of antibiotic treatment for chronic sinusitis is controversial. Special types of antibiotics may be used, and treatment may be needed for a longer time.
- In some severe cases or in cases where there is severe nasal congestion and inflammation, a short course of oral steroids are given to decrease swelling and improve sinus drainage. This treatment is generally very effective.
- Antifungal medications are not recommended.
Emergency Treatment
Emergency care is required if infection spreads beyond the nasal sinuses into the bone, brain, or other parts of the skull. High-dose antibiotics are administered intravenously, and emergency surgery is almost always necessary in such cases.
Lifestyle Changes
Hydration
Home remedies that open and hydrate the sinuses are often the only treatment necessary for mild sinusitis that is not accompanied by signs of acute infection.
Drinking plenty of fluids and getting lots of rest is still the best advice for easing mild symptoms:
- Water is the best fluid because it helps lubricate the mucous membranes. (There is no evidence that drinking milk will increase or worsen mucus, although milk is a food and should not serve as fluid replacement.)
- Chicken soup helps with congestion and aches. The hot steam from the soup may be its chief advantage, although other ingredients in the soup may have anti-inflammatory effects. In fact, any hot beverage may have similar soothing effects from steam. Ginger tea or any hot tea with honey and lemon can be helpful.
- Spicy foods that contain hot peppers or horseradish may help clear sinuses.
- Inhaling steam 2 to 4 times a day is extremely helpful, costs nothing, and requires no expensive equipment. Sit comfortably and lean over a bowl of hot water (no one should ever inhale steam from water as it boils) while covering the head and the bowl with a towel so the steam remains under the cloth. The steam should be inhaled continuously for 10 minutes. A mentholated or other aromatic preparation may be added to the water. Long, steamy showers, vaporizers, and facial saunas are alternatives.
Nasal Wash
A nasal wash can be helpful for removing mucus from the nose and relieving sinusitis symptoms. A saline (salt water) solution can be purchased in a spray bottle at a drug store or made at home. (Mix 1 teaspoon of table, Kosher, or sea salt with 2 cups of warm water. Some people add a pinch of baking soda.) If you prepare your own saline solution, it is not necessary to use bottled or boiled water; plain tap water is fine. Perform the nasal wash several times a day.
A simple method for administering a nasal wash is:
- Lean over the sink head down.
- Pour some solution into the palm of the hand and inhale it through the nose, one nostril at a time.
- Spit out the remaining solution.
- Gently blow the nose.
Neti pots have also become popular in recent years for prevention and treatment of sinusitis. To do nasal irrigation with a saline solution through a Neti pot:
- Lean over the sink with your head tilted to one side.
- Insert the spout of the Neti pot into the upper nostril.
- Slowly pour the salt water into your nose while continuing to breathe through your mouth.
- The water will flow through the upper nostril and out through the lower nostril.
- When the water finishes dripping out, blow your nose.
- Reverse the tilt of your head and repeat the process with the other nostril.
You can also use either a bulb syringe or a sinus rinse squeeze bottle sold at most pharmacies which provides more vigorous irrigations to break up thick, sticky mucous that often accompanies chronic infection.
Medications
Antibiotics
Antibiotic drugs are used to treat bacterial, not viral, infections. Unfortunately, because of the overuse and improper use of antibiotics, many types of bacteria no longer respond to antibiotic treatment. The bacteria have become resistant to these drugs.
Amoxicillin, a type of penicillin, is the main antibiotic used for mild-to-moderate acute bacterial sinusitis, but due to bacterial resistance it has become less effective. Amoxicillin-clavulanate (Augmentin, generic) may be used as an alternative to amoxicillin. It is a type of penicillin that works against a wide spectrum of bacteria.
People who have a history of penicillin allergy cannot take amoxicillin or amoxicillin-clavulanate. They will need to take another type of antibiotic such as doxycycline or levofloxacin.
Side effects of antibiotics may include:- Upset stomach.
- Vaginal infections (taking supplements of acidophilus or eating yogurt with active cultures may help restore healthy bacteria that offset the risk for such infections)
- Interactions with certain drugs, including some over-the-counter medications. Inform your doctor of all medications you are taking and of any drug allergies.
- Allergic reactions can range from mild skin rashes to rare but severe, and even life-threatening anaphylactic shock.
Corticosteroids
Nasal-spray corticosteroids, commonly called nasal steroid sprays, help reduce inflammation and mucus production. They may take up to several weeks of use to have an effect.
Corticosteroids that are available in nasal spray form and are approved for treating nasal allergy symptoms include:
- Triamcinolone (Nasacort Allergy HR)
- Mometasone furoate (Nasonex)
- Fluticasone (Flonase)
- Beclomethasone (Beconase, Vancenase), flunisolide (Nasalide), and budesonide (Rhinocort)
- These nasal sprays are also approved for children (ages vary depending on brand)
Side effects of nasal corticosteroids may include:
- Dryness, burning, stinging in the nasal passage
- Headache
- Nosebleed (inform your health care provider)
When taking a nasal steroid spray, it is very important that you direct the tip of the bottle towards the cheek or eye on that side of the face. This will direct the medicine towards the swollen glands and sinus passages and away from the central septum or cartilage which can be the source of nosebleeds. Also, do not sniff in deeply while using the spray because this directs all the medicine into the back of your nose and into your mouth instead of keeping it inside the nose where it should be.
Decongestants
Decongestants are drugs that help reduce nasal congestion. They are available in both pill and nasal spray forms. However, decongestants will not cure sinusitis. They may actually worsen sinusitis by increasing sinus inflammation if used too long. Nasal spray decongestants should not be used for more than 3 days in a row.
Due to the lack of evidence for the benefit of nasal decongestants in treating sinusitis, the FDA ordered manufacturers of over-the-counter (OTC) nasal decongestant products to remove all references to sinusitis from their labeling. The Infectious Diseases Society of America does not recommend nasal or oral decongestants for patients with acute bacterial sinusitis.
Your health care provider may still recommend that you take either an OTC or prescription nasal decongestant to help relieve blockage symptoms associated with sinusitis. If you think you have sinusitis, check with your provider before taking a decongestant.
Decongestants should never be used in infants and children under age 4, and some doctors recommend not giving them to children under age 14. Children are at particular risk for central nervous system side effects, including convulsions, rapid heart rate, loss of consciousness, and death.
Antihistamines
Antihistamines such as diphenhydramine (Benadryl, generic) are included in many cold and allergy medications. Because they dry and thicken nasal secretions, they make sinus drainage difficult and may worsen sinusitis. In general, people with sinusitis should not take antihistamines.
Surgery
Surgery can unblock the sinuses when drug therapy is not effective or if there are other complications, such as structural abnormalities or fungal sinusitis.
Functional Endoscopic Sinus Surgery
Functional endoscopic sinus surgery (FESS) is the standard procedure for most people who require surgical management of chronic sinusitis or polyposis. The procedure allows correction of obstructions, including polyps, ventilation, and drainage to aid healing.
Candidates for the Procedure: In general, surgery is reserved for people who have tried and failed medical therapy, including several courses of broad-spectrum antibiotics, nasal corticosteroids, and sinus drainage (when appropriate).People who may benefit from sinus surgery include those with:
- Nasal or sinus polyps who have not responded to intranasal or oral corticosteroids
- Congenital anatomic abnormalities
- Evidence of bone involvement
- HIV/AIDS or other immune system impairments who have chronic or recurrent sinusitis
- Adults and children need a general anesthetic.
- Before the procedure, a computed tomography (CT) scan is taken to help the surgeon plan the procedure and to guide the surgery.
- A rigid sinus endoscope that has a light and camera head attached are inserted through the nostrils to visualize the anatomy of the nose and sinuses.
- The surgeon uses special instruments to remove diseased bone or tissue and clear obstructions. Shavers are used to gently remove soft tissue such as polyps. Miniature bone cutters are sometimes used to open the floor of the frontal sinus and restore drainage.
- In some milder cases where the anatomy is not severely obstructed, a procedure called "Balloon sinuplasty" is performed in which a catheter with an inflatable balloon is used to enlarge the natural opening of one or more sinuses. Your surgeon will determine which one is the best surgery for you depending on your history and anatomy.
Postsurgical care involves the following:
- You will experience a dull ache around the nose and sinus cavity that can be treated with pain medication.
- Following surgery, you should flush the sinuses twice daily with a saline or alkaline solution.
- Antibiotics may be prescribed for several weeks until postnasal drip has stopped. Corticosteroid sprays and antihistamines may be needed.
Balloon Sinuplasty
A newer type of surgical procedure threads a small balloon through the sinus passages. As the balloon is gently opened, the sinus passages expand, allowing drainage to occur.
This procedure is best suited for select people with sinusitis disease in the maxillary (behind the cheekbones), frontal (behind the sides of the forehead), and sphenoid (behind the eyes) sinus regions. It is inappropriate for people with disease in the ethmoid (between the eyes) sinuses because of the risk of eye injury.
Invasive Conventional Surgery
Endoscopy is now used in most cases of chronic sinusitis, but in severe cases, invasive surgery using conventional scalpel techniques may be required to remove infected areas. This may be the case with acute ethmoid sinusitis in which pus breaks through the sinus and threatens the eye, very severe frontal sinusitis, invasive fungal sinusitis, or when cancer is present in the sinuses.
Resources
- www.entnet.org -- American Academy of Otolaryngology - Head and Neck Surgery
- www.aaaai.org -- American Academy of Allergy, Asthma, and Immunology
- www.acaai.org -- American College of Allergy, Asthma, and Immunology
- www.niaid.nih.gov -- National Institute of Allergy and Infectious Disease
- www.idsociety.org -- Infectious Diseases Society of America
- www.aap.org -- American Academy of Pediatrics
- www.american-rhinologic.org -- American Rhinologic Society
References
Ahovuo-Saloranta A, Rautakorpi UM, Borisenko OV, Liira H, Williams JW Jr, Mäkelä M. Antibiotics for acute maxillary sinusitis in adults. Cochrane Database Syst Rev . 2014 Feb 11;2:CD000243.
Ah-See KL, MacKenzie J, Ah-See KW. Management of chronic rhinosinusitis. BMJ . 2012;345:e7054.
Anon JB. Upper respiratory infections. Am J Med . 2010;123(4 Suppl):S16-S25.
Benninger MS, Stokken JK. Acute rhinosinusitis. In: Flint PW, ed. Cummings Otolaryngology . 6th ed. Elsevier Saunders; 2015:chap 46.
Chow AW, Benninger MS, Brook I, et al. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis . 2012;54(8):e72-e112.
DeMuri GP, Wald ER. Clinical practice: acute bacterial sinusitis in children. N Engl J Med . 2012;367(12):1128-1134.
DeMuri GP. Wald ER. Sinusitis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases . 8th ed. Elsevier Saunders; 2015:chap 63.
Dykewicz MS, Hamilos DL. Rhinitis and sinusitis. J Allergy Clin Immunol . 2010;125(2 Suppl 2):S103-S115.
Hamilos DL. Chronic rhinosinusitis: epidemiology and medical management. J Allergy Clin Immunol . 2011;128(4):693-707; quiz 708-709.
Hersh AL, Jackson MA, Hicks LA; American Academy of Pediatrics Committee on Infectious Diseases. Principles of judicious antibiotic prescribing for upper respiratory tract infections in pediatrics. Pediatrics . 2013;132(6):1146-54. Epub 2013 Nov 18.
Jarvis D, Newson R, Lotvall J, et al. Asthma in adults and its association with chronic rhinosinusitis: the GA2LEN survey in Europe. Allergy . 2012;67(1):91-98.
Rabago D, Zgierska A. Saline nasal irrigation for upper respiratory conditions. Am Fam Physician . 2009;80(10):1117-1119.
Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, Brook I, Kumar KA, Kramper M, et al. Clinical practice guideline (update): adult sinusitis executive summary. Otolaryngol Head Neck Surg . 2015 Apr;152(4):598-609.
Wald ER, Applegate KE, Bordley C, Darrow DH, Glode MP, Marcy SM, et al. Clinical practice guideline for the diagnosis and management of acute bacterial sinusitis in children aged 1 to 18 years. Pediatrics . Published online June 24, 2013.
Venekamp RP, Thompson MJ, Hayward G, Heneghan CJ, Del Mar CB, Perera R, et al. Systemic corticosteroids for acute sinusitis. Cochrane Database Syst Rev . 2014;3:CD008115.
Zalmanovici Trestioreanu A(1), Yaphe J. Intranasal steroids for acute sinusitis. Cochrane Database Syst Rev. 2013;12:CD005149.
Review Date: 6/29/2015
Reviewed By: Sumana Jothi MD, Specialist in Laryngology, Clinical Instructor UCSF Otolaryngology, NCHCS VA, SFVA, San Francisco, CA. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team. Author: Julia Mongo, MS.