Leishmaniasis
Kala-azar; Cutaneous leishmaniasis; Visceral leishmaniasis; Old world leishmaniasis; New world leishmaniasis
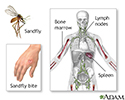
Leishmaniasis is an infectious disease spread by the bite of the female sandfly.
Causes
Leishmaniasis is caused by a tiny parasite called leishmania protozoa. Protozoa are one-celled organisms.
There are different forms of leishmaniasis.
- Cutaneous leishmaniasis affects the skin and mucous membranes. Skin sores usually start at the site of the sandfly bite. In a few people, sores may develop on mucous membranes.
- Systemic, or visceral, leishmaniasis affects the entire body. This form occurs 2 to 8 months after a person is bitten by the sandfly. Most people do not remember having a skin sore. This form can lead to deadly complications. The parasites damage the immune system by decreasing the numbers of disease-fighting cells.
Cases of leishmaniasis have been reported on all continents except Australia and Antarctica. In the Americas, leishmaniasis can be found in Mexico and South America. Leishmaniasis has been reported in military personnel returning from the Persian Gulf.
Symptoms
Symptoms of cutaneous leishmaniasis depend on where the lesions are located and may include:
- Breathing difficulty
- Skin sores, which may become a skin ulcer that heals very slowly
- Stuffy nose, runny nose, and nosebleeds
- Swallowing difficulty
- Ulcers and wearing away (erosion) in the mouth, tongue, gums, lips, nose, and inner nose
Systemic visceral infection in children usually begins suddenly with:
- Cough
- Diarrhea
- Fever
-
Vomiting
Vomiting
Nausea is feeling an urge to vomit. It is often called "being sick to your stomach. "Vomiting or throwing-up is forcing the contents of the stomach ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Adults usually have a fever for 2 weeks to 2 months, along with symptoms such as fatigue , weakness , and appetite loss. Weakness increases as the disease gets worse.
Fatigue
Fatigue is a feeling of weariness, tiredness, or lack of energy.
Other symptoms of systemic visceral leishmaniasis may include:
- Abdominal discomfort
- Fever that lasts for weeks; may come and go in cycles
- Night sweats
- Scaly, gray, dark, ashen skin
- Thinning hair
- Weight loss
Exams and Tests
Your health care provider will examine you and may find that your spleen, liver, and lymph nodes are enlarged. You will be asked if you recall being bitten by sandflies or if you've been in an area where leishmaniasis is common.
Tests that may be done to diagnose the condition include:
-
Biopsy
of the spleen and culture
Biopsy
A biopsy is the removal of a small piece of tissue for laboratory examination.
Read Article Now Book Mark Article -
Bone marrow biopsy
and culture
Bone marrow biopsy
A bone marrow biopsy is the removal of marrow from inside bone. Bone marrow is the soft tissue inside bones that helps form blood cells. It is foun...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Direct agglutination assay
- Indirect immunofluorescent antibody test
- Leishmania-specific PCR test
-
Liver biopsy
and culture
Liver biopsy
A liver biopsy is a test that takes a sample of tissue from the liver for examination.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Lymph node biopsy
and culture
Lymph node biopsy
A lymph node biopsy is the removal of lymph node tissue for examination under a microscope. The lymph nodes are small glands that make white blood ce...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Montenegro skin test (not approved in the United States)
-
Skin biopsy
and culture
Skin biopsy
A skin lesion biopsy is when a small amount of skin is removed so it can be examined. The skin is tested to look for skin conditions or diseases. A...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Other tests that may be done include:
-
Complete blood count
Complete blood count
A complete blood count (CBC) test measures the following:The number of red blood cells (RBC count)The number of white blood cells (WBC count)The tota...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Serologic testing
-
Serum albumin
Serum albumin
Albumin is a protein made by the liver. A serum albumin test measures the amount of this protein in the clear liquid portion of the blood. Albumin c...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Serum immunoglobulin levels
Serum immunoglobulin levels
Serum immunoelectrophoresis is a lab test that measures proteins called immunoglobulins in the blood. Immunoglobulins are proteins that function as ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Serum
protein
Protein
Proteins are the building blocks of life. Every cell in the human body contains protein. The basic structure of protein is a chain of amino acids. ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
Medicines called antimony-containing compounds are the main drugs used to treat leishmaniasis. These include:
- Meglumine antimoniate
- Sodium stibogluconate
Other drugs that may be used include:
- Amphotericin B
- Ketoconazole
- Miltefosine
- Paromomycin
- Pentamidine
Plastic surgery may be needed to correct the disfigurement caused by sores on the face (cutaneous leishmaniasis).
Outlook (Prognosis)
Cure rates are high with the proper medicine, especially when treatment is started before the immune system is damaged. Cutaneous leishmaniasis may lead to disfigurement.
Death is usually caused by complications (such as other infections), rather than from the disease itself. Death often occurs within 2 years.
Possible Complications
Leishmaniasis may lead to the following:
- Bleeding (hemorrhage)
- Deadly infections due to immune system damage
- Disfigurement of the face
When to Contact a Medical Professional
Contact your provider if you have symptoms of leishmaniasis after visiting an area where the disease is known to occur.
Prevention
Taking measures to avoid sandfly bites can help prevent leishmaniasis:
- Putting fine mesh netting around the bed (in areas where the disease occurs)
- Screening windows
- Wearing insect repellent
- Wearing protective clothing
Public health measures to reduce sandflies are important. There are no vaccines or drugs that prevent leishmaniasis.
References
Boelaert M, Sundar S. Leishmaniasis. In: Farrar J, Hotez PJ, Junghanss T, Kang G, Lalloo D, White NJ, eds. Manson's Tropical Diseases . 23rd ed. Philadelphia, PA: Elsevier Saunders; 2014:chap 47.
Magill AJ. Leishmania species. In: Bennett JE, Dolin R, Blaser MJ, eds. M andell, Douglas, and Bennett's Principles and Practice of Infectious Diseases . 8th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 277.
-
Leishmaniasis - illustration
Leishmaniasis is a parasitic disease spread by the bite of the sandfly and can cause skin disease and systemic disease. The systemic form can be fatal, but treatment with antimony-containing compounds produces a high cure rate.
Leishmaniasis
illustration
-
Leishmaniasis, mexicana - lesion on the cheek - illustration
Parasites are deposited in the skin by the bite of a sand-fly. These parasites (leishmania) produce a local sore at the site of the bite and migrate throughout the body, causing tissue destruction at distant sites.
Leishmaniasis, mexicana - lesion on the cheek
illustration
-
Leishmaniasis on the finger - illustration
Leishmaniasis is seen in the United States mainly in people who have traveled outside the U.S. There are several different types of leishmaniasis, but all are transmitted by the bite of a sandfly. An initial sore develops at the site of the bite, as shown here. The infection may spread through the body from that point.
Leishmaniasis on the finger
illustration
-
Leishmania panamensis on the foot - illustration
Leishmaniasis is seen in the United States mainly in people who have traveled outside the U.S. There are several different types of leishmaniasis, but all are transmitted by the bite of a sandfly. An initial sore develops at the site of the bite, as shown here. The infection may spread through the body from that point.
Leishmania panamensis on the foot
illustration
-
Leishmania panamensis - close-up - illustration
Leishmaniasis is seen in the United States mainly in people who travel outside the U.S. There are several different types of leishmaniasis, but all are transmitted by the bite of a sandfly. This is the typical appearance of the early stage of leishmaniasis.
Leishmania panamensis - close-up
illustration
-
Leishmaniasis - illustration
Leishmaniasis is a parasitic disease spread by the bite of the sandfly and can cause skin disease and systemic disease. The systemic form can be fatal, but treatment with antimony-containing compounds produces a high cure rate.
Leishmaniasis
illustration
-
Leishmaniasis, mexicana - lesion on the cheek - illustration
Parasites are deposited in the skin by the bite of a sand-fly. These parasites (leishmania) produce a local sore at the site of the bite and migrate throughout the body, causing tissue destruction at distant sites.
Leishmaniasis, mexicana - lesion on the cheek
illustration
-
Leishmaniasis on the finger - illustration
Leishmaniasis is seen in the United States mainly in people who have traveled outside the U.S. There are several different types of leishmaniasis, but all are transmitted by the bite of a sandfly. An initial sore develops at the site of the bite, as shown here. The infection may spread through the body from that point.
Leishmaniasis on the finger
illustration
-
Leishmania panamensis on the foot - illustration
Leishmaniasis is seen in the United States mainly in people who have traveled outside the U.S. There are several different types of leishmaniasis, but all are transmitted by the bite of a sandfly. An initial sore develops at the site of the bite, as shown here. The infection may spread through the body from that point.
Leishmania panamensis on the foot
illustration
-
Leishmania panamensis - close-up - illustration
Leishmaniasis is seen in the United States mainly in people who travel outside the U.S. There are several different types of leishmaniasis, but all are transmitted by the bite of a sandfly. This is the typical appearance of the early stage of leishmaniasis.
Leishmania panamensis - close-up
illustration
Review Date: 9/10/2015
Reviewed By: Jatin M. Vyas, MD, PhD, Assistant Professor in Medicine, Harvard Medical School; Assistant in Medicine, Division of Infectious Disease, Department of Medicine, Massachusetts General Hospital, Boston, MA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.