Pulmonary embolus
Venous thromboembolism; Lung blood clot; Blood clot - lung; Embolus; Tumor embolus; Embolism - pulmonary; DVT-pulmonary embolism; Thrombosis - pulmonary embolism
A pulmonary embolus is a blockage of an artery in the lungs. The most common cause of the blockage is a blood clot .
Blood clot
Blood clots are clumps that occur when blood hardens from a liquid to a solid. A blood clot that forms inside one of your veins or arteries is calle...

Causes
A pulmonary embolus is most often caused by a blood clot that develops in a vein outside the lungs. The most common blood clot is one in a deep vein of the thigh or in the pelvis (hip area). This type of clot is called a deep vein thrombosis (DVT) . The blood clot breaks off and travels to the lungs where it lodges.
Deep vein thrombosis (DVT)
Deep vein thrombosis (DVT) is a condition that occurs when a blood clot forms in a vein deep inside a part of the body. It mainly affects the large ...

Less common causes include air bubbles, fat droplets, amniotic fluid, or clumps of parasites or tumor cells.
You are more likely to get this condition if you or your family has a history of blood clots or certain clotting disorders. A pulmonary embolus may occur:
- After childbirth
- After heart attack, heart surgery, or stroke
- After severe injuries, burns, or fractures of the hips or thigh bone
- After surgery, most commonly bone, joint, or brain surgery
- During or after a long plane or car ride
- If you have cancer
- If you take birth control pills or estrogen therapy
- Long-term bed rest or staying in one position for a long time
Disorders that may lead to blood clots include:
-
Diseases of the immune system that make it
harder for the blood to clot
.
Harder for the blood to clot
Lupus anticoagulants are antibodies against substances in the lining of cells. These substances prevent blood clotting in a test tube. They are cal...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Inherited disorders that make the blood more likely to clot. One such disorder is
antithrombin III deficiency
.
Antithrombin III deficiency
Congenital antithrombin III deficiency is a genetic disorder that causes the blood to clot more than normal.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Symptoms
Main symptoms of a pulmonary embolism include chest pain that may be any of the following:
- Under the breastbone or on one side
- Sharp or stabbing
- Burning, aching, or a dull, heavy sensation
- Often gets worse with deep breathing
- You may bend over or hold your chest in response to the pain
Other symptoms may include:
- Bluish skin (cyanosis)
- Dizziness, lightheadedness, or fainting
- Fast breathing or wheezing
- Fast heart rate
- Feeling anxious
- Leg pain, redness, or swelling
- Low blood pressure
- Sudden cough, possibly coughing up blood or bloody mucus
- Shortness of breath that starts suddenly
- Sweating, clammy skin
Exams and Tests
The health care provider will perform a physical exam and ask about your symptoms and medical history.
The following lab tests may be done to see how well your lungs are working:
-
Arterial
blood gases
Blood gases
Blood gases are a measurement of how much oxygen and carbon dioxide are in your blood. They also determine the acidity (pH) of your blood.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Pulse oximetry
The following imaging tests can help determine where the blood clot is located:
-
Chest x-ray
Chest x-ray
A chest x-ray is an x-ray of the chest, lungs, heart, large arteries, ribs, and diaphragm.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - CT angiogram of the chest
- Pulmonary ventilation/perfusion scan, also called a V/Q scan
-
Pulmonary angiogram
Pulmonary angiogram
Pulmonary angiography is a test to see how blood flows through the lung. Angiography is an imaging test that uses x-rays and a special dye to see in...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Other tests that may be done include:
- Chest CT scan
-
D-dimer blood test
D-dimer blood test
D-dimer tests are used to check for blood clotting problems. Blood clots can cause health problems, such as:Deep vein thrombosis (DVT)Pulmonary embo...
Read Article Now Book Mark Article -
Doppler ultrasound exam of the legs
Doppler ultrasound exam of the legs
This test uses ultrasound to look at the blood flow in the large arteries and veins in the arms and legs.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Echocardiogram
(ECG)
Echocardiogram
An echocardiogram is a test that uses sound waves to create pictures of the heart. The picture and information it produces is more detailed than a s...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Blood tests may be done to check if you have an increased chance of blood clotting, including:
- Antiphospholipid antibodies
- Genetic testing to look for changes that make you more likely to develop blood clots
- Lupus anticoagulant
- Protein C and protein S levels
Treatment
A pulmonary embolus requires treatment right away. You may need to stay in the hospital:
- You will receive medicines to thin the blood and make it less likely your blood will form more clots.
- In cases of severe, life-threatening pulmonary embolism, treatment may involve dissolving the clot. This is called thrombolytic therapy. You will receive medicines to dissolve the clot.
Whether or not you need to stay in the hospital, you will likely need to take medicines at home to thin the blood:
-
You may be given
pills to take
or you may need to give yourself injections.
Pills to take
Warfarin is a medicine that makes your blood less likely to form clots. This may be important if:You have already had blood clots in your leg, arm, ...
Read Article Now Book Mark Article - For some medicines, you will need blood tests to monitor your dosage.
- How long you need to take these medicines depends mostly on the cause and size of your blood clot.
- Your provider will talk to you about the risk of bleeding problems when you take these medicines.
If you cannot take blood thinners, your doctor may suggest surgery to place a device called an inferior vena cava filter (IVC filter). This device is placed in the main vein in your belly. It keeps large clots from traveling into the blood vessels of the lungs. Sometimes, a temporary filter can be placed and removed later.
Outlook (Prognosis)
How well a person recovers from a pulmonary embolus can be hard to predict. It often depends on:
- What caused the problem in the first place (for example, cancer, major surgery, or an injury)
- The size of the blood clot in the lungs
- If the blood clot dissolves over time
Some people can develop long-term heart and lung problems.
Death is possible in people with a severe pulmonary embolism.
When to Contact a Medical Professional
Go to the emergency room or call the local emergency number (such as 911), if you have symptoms of pulmonary embolus.
Prevention
Blood thinners may be prescribed to help prevent DVT in people at high risk, or those who are undergoing high-risk surgery.
If you had a DVT, your provider will prescribe pressure stockings. Wear them as instructed. They will improve blood flow in your legs and reduce your risk of blood clots.
Moving your legs often during long plane trips, car trips, and other situations in which you are sitting or lying down for long periods can also help prevent DVT. People at very high risk for blood clots may need shots of a blood thinner called heparin when they take a flight that lasts longer than 4 hours.
Do not smoke. If you smoke, quit. Women who are taking estrogen must stop smoking. Smoking increases your risk of developing blood clots.
References
Guyatt GH, Akl EA, Crowther M, et al. Executive summary: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest . 2012;141(2suppl):7s-47s. PMID: 22315257 www.ncbi.nlm.nih.gov/pubmed/22315257 .
Kline JA. Pulmonary embolism and deep vein thrombosis. In: Marx JA, Hockberger RS, Walls RM, et al, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice . 8th ed. Philadelphia, PA: Elsevier Saunders; 2014:chap 88.
Weitz JI. Pulmonary embolism. In: Goldman L, Schafer AI, eds. Goldman's Cecil Medicine . 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 98.
-
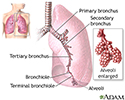
Lungs - illustration
The major features of the lungs include the bronchi, the bronchioles and the alveoli. The alveoli are the microscopic blood vessel-lined sacks in which oxygen and carbon dioxide gas are exchanged.
Lungs
illustration
-
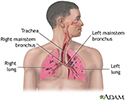
Respiratory system - illustration
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Respiratory system
illustration
-
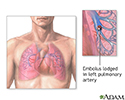
Pulmonary embolus - illustration
An embolus is a blockage of an artery in the lungs by fat, air, tumor tissue, or blood clot.
Pulmonary embolus
illustration
-
Lungs - illustration
The major features of the lungs include the bronchi, the bronchioles and the alveoli. The alveoli are the microscopic blood vessel-lined sacks in which oxygen and carbon dioxide gas are exchanged.
Lungs
illustration
-
Respiratory system - illustration
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Respiratory system
illustration
-
Pulmonary embolus - illustration
An embolus is a blockage of an artery in the lungs by fat, air, tumor tissue, or blood clot.
Pulmonary embolus
illustration
Review Date: 12/4/2015
Reviewed By: Yi-Bin Chen, MD, Leukemia/Bone Marrow Transplant Program, Massachusetts General Hospital, Boston, MA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.