Acute pancreatitis
Gallstone pancreatitis; Pancreas - inflammation
Acute pancreatitis is sudden swelling and inflammation of the pancreas.
Causes
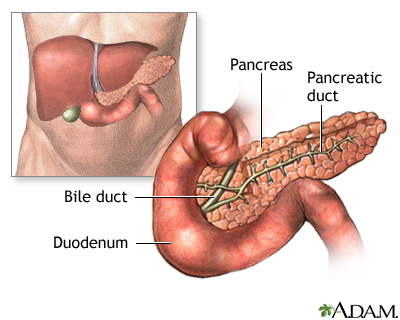
The pancreas is an organ located behind the stomach. It produces the hormones insulin and glucagon. It also produces chemicals called enzymes needed to digest food.
Most of the time, the enzymes are only active after they reach the small intestine.
- If these enzymes become active inside the pancreas, they can digest the tissue of the pancreas. This causes swelling, bleeding, and damage to the organ and its blood vessels.
- This problem is called acute pancreatitis.
Acute pancreatitis affects men more often than women. Certain diseases, surgeries, and habits make you more likely to develop this condition.
- Alcohol use is responsible for up to 70% of cases in the United States. About 5 to 8 drinks per day for 5 or more years can damage the pancreas.
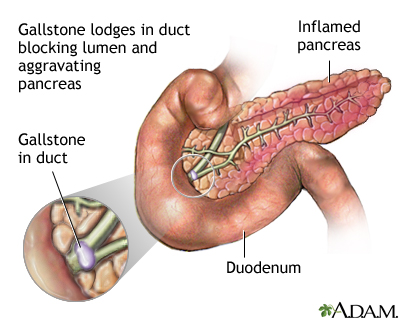
- Gallstones are the next most common cause. When the gallstones travel out of the gallbladder into the bile ducts, they block the opening that drains bile and enzymes. The bile and enzymes "back up" into the pancreas and cause swelling.
- Genetics may be a factor in some cases. Sometimes, the cause is not known.
Other conditions that have been linked to pancreatitis are:
- Autoimmune problems (when the immune system attacks the body)
- Damage to the ducts or pancreas during surgery
-
High blood levels of a fat called
triglycerides
-- most often above 1,000 mg/dL
Triglycerides
Familial hypertriglyceridemia is a common disorder passed down through families. It causes a higher-than-normal level of triglycerides (a type of fa...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Injury to the pancreas from an accident
Other causes include:
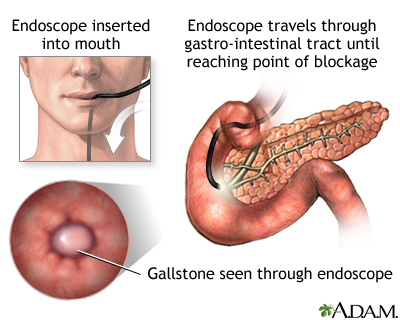
- After certain procedures used to diagnose gallbladder and pancreas problems (ERCP) or ultrasound guided biopsy
-
Cystic fibrosis
Cystic fibrosis
Cystic fibrosis is a disease that causes thick, sticky mucus to build up in the lungs, digestive tract, and other areas of the body. It is one of th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Overactive parathyroid gland
Overactive parathyroid gland
Hyperparathyroidism is a disorder in which the parathyroid glands in your neck produce too much parathyroid hormone (PTH).
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Reye syndrome
Reye syndrome
Reye syndrome is sudden (acute) brain damage and liver function problems. This condition does not have a known cause. This syndrome has occurred in ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Use of certain medicines (especially estrogens, corticosteroids, sulfonamides, thiazides, and azathioprine)
- Certain infections that involve the pancreas
Symptoms
The main symptom of pancreatitis is pain felt in the upper left side or middle of the abdomen. The pain :
Pain
Abdominal pain is pain that you feel anywhere between your chest and groin. This is often referred to as the stomach region or belly.

- May be worse within minutes after eating or drinking at first, more commonly if foods have a high fat content
- Becomes constant and more severe, lasting for several days
- May be worse when lying flat on the back
- May spread (radiate) to the back or below the left shoulder blade
People with acute pancreatitis often look ill and have a fever, nausea, vomiting, and sweating.
Other symptoms that may occur with this disease include:
- Clay-colored stools
-
Bloating and fullness
Bloating and fullness
Gas is air in the intestine that is passed through the rectum. Air that moves from the digestive tract through the mouth is called belching. Gas is ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Hiccups
Hiccups
A hiccup is an unintentional movement (spasm) of the diaphragm, the muscle at the base of the lungs. The spasm is followed by quick closing of the v...
Read Article Now Book Mark Article -
Indigestion
Indigestion
Indigestion (dyspepsia) is a mild discomfort in the upper belly or abdomen. It occurs during or right after eating. It may feel like:Heat, burning,...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Mild yellowing of the skin and whites of the eyes (jaundice)
-
Swollen abdomen
Swollen abdomen
A swollen abdomen is when your belly area is bigger than usual.
Read Article Now Book Mark Article
Exams and Tests
The health care provider will do a physical exam, which may show:
- Abdominal tenderness or lump (mass)
- Fever
-
Low blood pressure
Low blood pressure
Low blood pressure occurs when blood pressure is much lower than normal. This means the heart, brain, and other parts of the body do not get enough ...
Read Article Now Book Mark Article - Rapid heart rate
- Rapid breathing (respiratory) rate
Lab tests that show the release of pancreatic enzymes will be done. These include:
-
Increased blood amylase level
Increased blood amylase level
Amylase is an enzyme that helps digest carbohydrates. It is made in the pancreas and the glands that make saliva. When the pancreas is diseased or ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Increased
serum blood lipase level
Serum blood lipase level
Lipase is a protein (enzyme) released by the pancreas into the small intestine. It helps the body absorb fat. This test is used to measure the amou...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Increased
urine amylase level
Urine amylase level
This is a test that measures the amount of amylase in urine. Amylase is an enzyme that helps digest carbohydrates. It is produced mainly in the pan...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Other blood tests that can help diagnose pancreatitis or its complications include:
-
Complete blood count
(CBC)
Complete blood count
A complete blood count (CBC) test measures the following:The number of red blood cells (RBC count)The number of white blood cells (WBC count)The tota...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Comprehensive metabolic panel
Comprehensive metabolic panel
A comprehensive metabolic panel is a group of blood tests. They provide an overall picture of your body's chemical balance and metabolism. Metaboli...
Read Article Now Book Mark Article
Imaging tests that can show swelling of the pancreas include:
-
CT scan of the abdomen
CT scan of the abdomen
An abdominal CT scan is an imaging method. This test uses x-rays to create cross-sectional pictures of the belly area. CT stands for computed tomog...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
MRI of the abdomen
MRI of the abdomen
An abdominal magnetic resonance imaging scan is an imaging test that uses powerful magnets and radio waves. The waves create pictures of the inside ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Ultrasound of the abdomen
Ultrasound of the abdomen
Abdominal ultrasound is a type of imaging test. It is used to look at organs in the abdomen, including the liver, gallbladder, spleen, pancreas, and...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
Treatment often requires a stay in the hospital. It may involve:
- Pain medicines
- Fluids given through a vein (IV)
- Stopping food or fluid by mouth to limit the activity of the pancreas
A tube may be inserted through the nose or mouth to remove the contents of the stomach. This may be done if vomiting and severe pain do not improve. The tube will stay in for 1 to 2 days to 1 to 2 weeks.
Treating the condition that caused the problem can prevent repeated attacks.
In some cases, therapy is needed to:
-
Drain
fluid that has collected in or around the pancreas
Fluid that has collected in or around t...
A pancreatic pseudocyst is a fluid-filled sac in the abdomen. It may also contain tissue from the pancreas, enzymes, and blood.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Remove
gallstones
Gallstones
Gallstones are hard deposits that form inside the gallbladder. Gallstones may be as small as a grain of sand or as large as a golf ball.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Relieve blockages of the pancreatic duct
In the most severe cases, surgery is needed to remove damaged, dead or infected pancreatic tissue.
Avoid smoking, alcoholic drinks, and fatty foods after the attack has improved.
Outlook (Prognosis)
Most cases go away in a week. However, some cases develop into a life-threatening illness.
The death rate is high with:
-
Bleeding in the pancreas
has occurred
Bleeding in the pancreas
Hemorrhage is the medical term for bleeding. It usually refers to excessive bleeding. Hemorrhagic diseases are caused by bleeding, or they result i...
Read Article Now Book Mark Article - Liver, heart, or kidney problems are also present
- An abscess forms the pancreas
- There is death or necrosis of larger amounts of tissue in the pancreas
Sometimes the swelling and infection do not fully heal. Repeat episodes of pancreatitis may also occur. Either of these can lead to long-term damage of the pancreas .
Long-term damage of the pancreas
Pancreatitis is swelling of the pancreas. Chronic pancreatitis is present when this problem does not heal or improve, gets worse over time, and lead...

Possible Complications
Pancreatitis can return. The chances of it returning depend on the cause, and how well it can be treated. Complications of acute pancreatitis may include:
-
Acute kidney failure
Acute kidney failure
Acute kidney failure is the rapid (less than 2 days) loss of your kidneys' ability to remove waste and help balance fluids and electrolytes in your b...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Long-term lung damage
(ARDS)
Long-term lung damage
Acute respiratory distress syndrome (ARDS) is a life-threatening lung condition that prevents enough oxygen from getting to the lungs and into the bl...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Buildup of fluid in the abdomen (
ascites
)
Ascites
Ascites is the build-up of fluid in the space between the lining of the abdomen and abdominal organs.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Cysts
or
abscesses
in the pancreas
Cysts
A cyst is a closed pocket or pouch of tissue. It can be filled with air, fluid, pus, or other material.
Read Article Now Book Mark ArticleAbscesses
An abscess is a collection of pus in any part of the body. In most cases, the area around an abscess is swollen and inflamed.
Read Article Now Book Mark Article -
Heart failure
Heart failure
Heart failure is a condition in which the heart is no longer able to pump oxygen-rich blood to the rest of the body efficiently. This causes symptom...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
When to Contact a Medical Professional
Call your provider if:
- You have intense, constant abdominal pain.
- You develop other symptoms of acute pancreatitis.
Prevention
You may lower your risk of new or repeat episodes of pancreatitis by taking steps to prevent the medical conditions that can lead to the disease:
- DO NOT drink too much alcohol.
-
Make sure
children receive vaccines
to protect them against mumps and other childhood illnesses.
Children receive vaccines
Vaccines are used to boost your immune system and prevent serious, life-threatening diseases.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Treat medical problems that lead to high blood levels of triglycerides.
References
Forsmark CE. Pancreatitis. In: Goldman L, Schafer AI, eds. Goldman's Cecil Medicine . 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 144.
Tenner S, Baillie J, DeWitt J, et al. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol . 2013;108:1400-1415. PMID: 23896955 www.ncbi.nlm.nih.gov/pubmed/23896955 .
Tenner S, Steinbert WM. Acute pancreatitis. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger & Fordtran's Gastrointestinal and Liver Disease . 10th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 58.
-
Digestive system - illustration
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
Digestive system
illustration
-
Endocrine glands - illustration
Endocrine glands release hormones (chemical messengers) into the bloodstream to be transported to various organs and tissues throughout the body. For instance, the pancreas secretes insulin, which allows the body to regulate levels of sugar in the blood. The thyroid gets instructions from the pituitary to secrete hormones which determine the pace of chemical activity in the body (the more hormone in the bloodstream, the faster the chemical activity; the less hormone, the slower the activity).
Endocrine glands
illustration
-
Pancreatitis, acute - CT scan - illustration
This upper abdominal CT scan shows inflammation and swelling of the pancreas caused by acute infection (pancreatitis).
Pancreatitis, acute - CT scan
illustration
-
Normal anatomy
Presentation
-
Digestive system - illustration
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
Digestive system
illustration
-
Endocrine glands - illustration
Endocrine glands release hormones (chemical messengers) into the bloodstream to be transported to various organs and tissues throughout the body. For instance, the pancreas secretes insulin, which allows the body to regulate levels of sugar in the blood. The thyroid gets instructions from the pituitary to secrete hormones which determine the pace of chemical activity in the body (the more hormone in the bloodstream, the faster the chemical activity; the less hormone, the slower the activity).
Endocrine glands
illustration
-
Pancreatitis, acute - CT scan - illustration
This upper abdominal CT scan shows inflammation and swelling of the pancreas caused by acute infection (pancreatitis).
Pancreatitis, acute - CT scan
illustration
-
Normal anatomy
Presentation
Review Date: 10/27/2015
Reviewed By: Subodh K. Lal, MD, gastroenterologist with Gastrointestinal Specialists of Georgia, Austell, GA. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.